Related Articles
- 15 Jun 21
Medium-chain triglycerides, or MCTs, have been popularized in the context of Bulletproof™ coffee or the ketogenic diet. MCTs and the keto diet have been investigated in the management of obesity, insulin resistance, , epilepsy, neurodegenerative conditions, and others.
- 12 Feb 20
Mild traumatic brain injuries (mTBIs) and postconcussion syndrome are becoming more of a public health concern. Although termed “mild,” the effects can certainly be debilitating and severe in some cases. The symptoms of postconcussion syndrome include headaches, memory and concentration difficulties, irritability, fatigue, nausea, visual disturbances, light and noise sensitivity, judgement problems, depression, and anxiety.
- 10 Jun 20
Peripheral neuropathy is a common type of neuralgia, with diabetic neuropathy and postherpetic neuralgia being the most common types.
- 09 Jan 20
There are various supports for headache management such as supplements, acupuncture/body work, and herbal medicine.
Headaches can be divided into different categories, determining treatment type. - 08 Jul 20
As the COVID-19 pandemic seemed to shut down the world, grocery stores, or at least what was left on the shelves at grocery stores, became an indicator of where people were at in their experience of the stressful event.
- 17 Aug 16
- 01 Feb 14
With the growing prevalence of cognitive decline, there is a need for sustainable lifestyle interventions to support, maintain, and improve cognitive health. As physical exercise bolsters bodily health, so too is there a need for mental training. The evolution of technology offers new, promising mediums for cognitive training. This medium is the realm of virtual reality, video games, and mobile devices, that allow for the development of individualized training regimes tailored to suit the person’s needs.
- 13 Apr 17
- 08 Jun 15
- 08 Jun 15
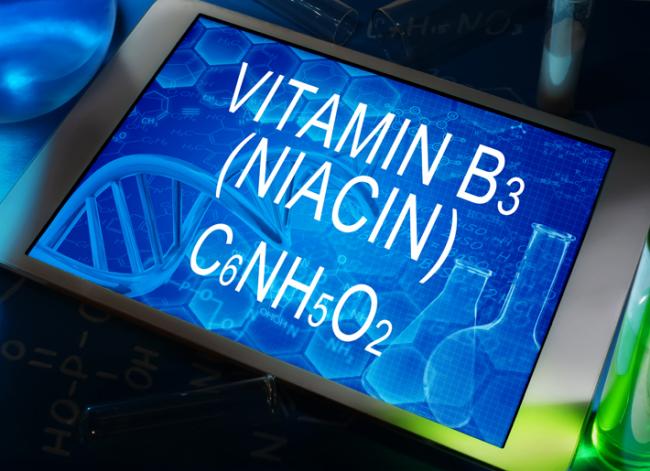
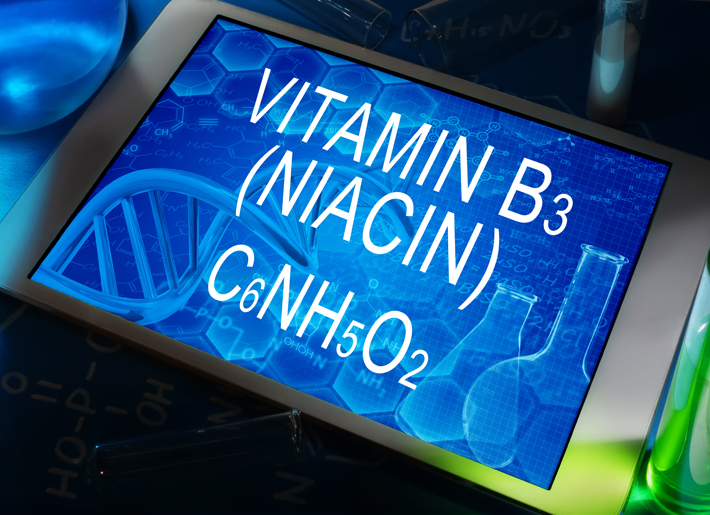 Niacin is one form of vitamin B3. Niacinamide and inositol hexanicotinate are the other two forms of B3 that exist; these forms are generally used to treat different conditions within the body. B vitamins ultimately help the body utilize fats and proteins; they also help convert food into fuel which is then used to produce energy.
Niacin is one form of vitamin B3. Niacinamide and inositol hexanicotinate are the other two forms of B3 that exist; these forms are generally used to treat different conditions within the body. B vitamins ultimately help the body utilize fats and proteins; they also help convert food into fuel which is then used to produce energy. - 22 Dec 15
 Our eyes and our sense of vision are extremely important to quality of life. As we age, our eyes tend to deteriorate, not only with regards to acuity, but also with regards to overall health. There are two conditions which are quite common and both cause problems with vision. These conditions are presented below.
Our eyes and our sense of vision are extremely important to quality of life. As we age, our eyes tend to deteriorate, not only with regards to acuity, but also with regards to overall health. There are two conditions which are quite common and both cause problems with vision. These conditions are presented below. - 13 Feb 16
Restless leg syndrome (RLS) is a condition that affects the part of the nervous system that causes an urge to move the legs. It usually interferes with sleep, so it can also be considered a sleep disorder. RLS can be quite troubling depending on the intensity of the symptoms. Symptoms include itching, burning, aching, and a desire to move the legs (for no apparent reason).
- 17 Jun 16
 The use of complementary medicine for the treatment of cancer and its side effects has skyrocketed in recent years. Complementary therapies refer to ones that are nonpharmaceutical in nature, and that have the potential to not only enhance quality of life, but also to reduce side effects of conventional therapy.
The use of complementary medicine for the treatment of cancer and its side effects has skyrocketed in recent years. Complementary therapies refer to ones that are nonpharmaceutical in nature, and that have the potential to not only enhance quality of life, but also to reduce side effects of conventional therapy. - 09 Jul 15
 W. somnifera, also known as Ashwagandha, is an important herb that has been used for over 3000 years. The important constituents of the root are steroidal alkaloids and steroidal lactones referred to as withanolides. It is used for anxiety, inflammation, Parkinson’s disease, cognitive and neurological disorders, and as a supportive adjunct for people undergoing radiation and chemotherapy.
W. somnifera, also known as Ashwagandha, is an important herb that has been used for over 3000 years. The important constituents of the root are steroidal alkaloids and steroidal lactones referred to as withanolides. It is used for anxiety, inflammation, Parkinson’s disease, cognitive and neurological disorders, and as a supportive adjunct for people undergoing radiation and chemotherapy. - 09 Jul 15
 Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank.
Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank. - 02 Nov 16
- 08 Jan 15
Tinnitus is the medical term used to describe “ringing in the ears.” Tinnitus is defined as the conscious perception of an auditory sensation in the absence of an external stimulus. Tinnitus is a rather common symptom that can be quite persistent and therefore disruptive to daily activities and quality of life. The extent of debility, however, can vary from one person to the next.
- 06 Nov 14
 S-Adenosylmethionine (SAMe) is a molecule that is distributed widely throughout the body and is crucial in a number of biochemical reactions. SAMe first garnered research attention in the 1970s, and has been used as an antidepressant in Europe since that time. However it has not become available in North America until the last 15 years or so. Biochemically, SAMe functions as a methyl-group donor, and works in the same pathways as folic acid and vitamin B12.
S-Adenosylmethionine (SAMe) is a molecule that is distributed widely throughout the body and is crucial in a number of biochemical reactions. SAMe first garnered research attention in the 1970s, and has been used as an antidepressant in Europe since that time. However it has not become available in North America until the last 15 years or so. Biochemically, SAMe functions as a methyl-group donor, and works in the same pathways as folic acid and vitamin B12. - 17 Aug 16
Chronic fatigue syndrome (CFS) is a chronic condition that can be difficult to diagnose and treat. It is a condition where extreme fatigue cannot be explained by any medical condition. It can get worse with mental or physical activity, but does not usually get better with rest...
- 08 Jan 15
 Vertigo is the feeling that your surroundings are moving when in reality they are still. Symptoms include feeling off-balance or feeling like the room is spinning. If it’s severe, there may be nausea and vomiting associated with it, and there could be an increased risk of falling. Vertigo can last for a few minutes or even days. Vertigo needs to be differentiated from feeling light-headed, which is usually due to a lack of circulation to the brain or due to low blood pressure. Feeling light-headed can also cause dizziness, but it is treated differently (it is suggested you lie down, that way you help the blood get back to your brain).
Vertigo is the feeling that your surroundings are moving when in reality they are still. Symptoms include feeling off-balance or feeling like the room is spinning. If it’s severe, there may be nausea and vomiting associated with it, and there could be an increased risk of falling. Vertigo can last for a few minutes or even days. Vertigo needs to be differentiated from feeling light-headed, which is usually due to a lack of circulation to the brain or due to low blood pressure. Feeling light-headed can also cause dizziness, but it is treated differently (it is suggested you lie down, that way you help the blood get back to your brain).
Newsletter
Most Popular
- 09 Nov 15
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13