Related Articles
- 12 Feb 20
Endometriosis is one of the most common chronic gynecological conditions in women of reproductive age. Not only is it associated with severe, debilitating pain, but it can also have significant implications for a woman’s fertility.[1]
- 09 Mar 20
Seasonal affective disorder (SAD) is a type of depression that is only present during the winter months. This differs from clinical depression, which has no seasonal pattern. SAD also tends to improve when the springtime occurs.
- 28 Jan 21Advanced glycation end-products (AGEs) are compounds that are generated under hyperglycemic conditions. They could be formed endogenously, or they could be consumed from our diet. Increased presence of AGEs in the human body is associated with diverse age-related and chronic conditions...
- 13 Apr 20
Bone is our main structural support system. It allows us to protect our vital organs, facilitates movement, and creates a scaffold for blood vessels and nerves. In additional to the structural functions, bone has important metabolic and endocrine functions as well.
- 12 Feb 20
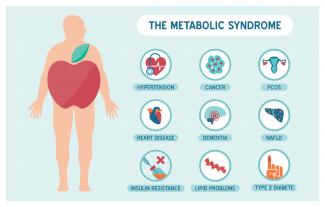
Metabolic syndrome is a cluster of risk factors that increase one’s chances of developing serious illnesses in the future. Metabolic syndrome doubles the chance of developing cardiovascular disease while increasing the risk of diabetes, fatty liver, and several types of cancers.[1][2]
- 13 Apr 20
Although it has been fraught with debate, and even disdain on occasion, the use of airbrushing of photos emanating from the marketing world of skin care and beauty tells us one thing: our society has a desire for evenness in skin appearance.
- 09 Jan 20
Premenstrual symptoms affect up to 80% of women. For many, these symptoms are bothersome but do not necessarily impact their daily functioning. Premenstrual syndrome (PMS), however, affects up to 20% of women. This diagnosis is defined by a woman’s experience of at least one physical and one psychiatric symptom each month in the second half of her cycle (7–14 days before her period), that alleviate with or shortly after the onset of menses.
- 10 Jun 20
Depression and anxiety deplete your energy, desire, and hope. They make it difficult for you to take a step that can help you to feel better. Depression is the second most frequent medical condition seen in common medical practice around the world; it is caused by alterations of the neurotransmitters in our central nervous system.[1] It is a mood disorder that occurs differently in different individuals.
- 12 Feb 20
Mild traumatic brain injuries (mTBIs) and postconcussion syndrome are becoming more of a public health concern. Although termed “mild,” the effects can certainly be debilitating and severe in some cases. The symptoms of postconcussion syndrome include headaches, memory and concentration difficulties, irritability, fatigue, nausea, visual disturbances, light and noise sensitivity, judgement problems, depression, and anxiety.
- 09 Mar 20
The viruses that cause colds and the flu can be spread easily by coughing and sneezing. While there is no way to guarantee you won’t get sick this winter, there are things you can do to reduce the severity of your sickness.
- 10 Jun 20
Peripheral neuropathy is a common type of neuralgia, with diabetic neuropathy and postherpetic neuralgia being the most common types.
- 08 Jul 20
Anxiety is a very common mental-health disorder and can have implications on all aspects of one’s life. This may come from a variety of factors such as finances, relationships, health, and more. Anxiety lends itself well to natural treatments such as herbal medicine, supplements, and lifestyle modification
- 09 Jan 20
There are various supports for headache management such as supplements, acupuncture/body work, and herbal medicine.
Headaches can be divided into different categories, determining treatment type. - 13 Apr 20
Itchy skin, dryness, redness, and cracking—uncomfortable signs of an eczema flare-up that can range from mild to having a significant impact on quality of life. Corticosteroid creams can do a fine job of targeting symptoms and inflammation associated with eczema, although below are some suggestions to get to the root cause and prevent future flare-ups.
- 07 Aug 20
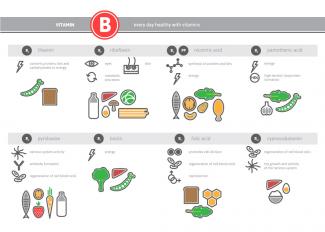
We know that vitamins play an important role in our energy and daily metabolic functions. We know that eating a balanced diet full of fruits and vegetables can help lower the risk of chronic disease and support brain functions. B vitamins are crucial to brain health and can reduce the intensity of mental illness, including symptoms relating to anxiety, depression, and chronic fatigue.
- 08 Jul 20
Hormones are essential signaling molecules in the body, but can create extreme pain and discomfort for women if they are out of balance. Premenstrual syndrome (PMS) has been the brunt of many jokes over many decades. However, the truth of this syndrome can be devastating for the sufferer, her relationships and her career.
- 08 Jul 20
Polycystic ovarian syndrome (PCOS) is one of the most common endocrine disorders. PCOS affects one in every five women of the reproductive age.
- 26 Feb 21
The kidneys are one of the body’s most important filtration systems and are sometimes overlooked until there is an issue. In traditional Chinese medicine, the kidneys are often referred to as the “root of life,” and they play an important role in overall vitality, especially as we age.
- 27 Apr 22
One of the key tenants of naturopathic medicine is education. In fact, one of the guiding principles of Naturopathic Medicine is Doctor as Teacher . This principle highlights the empowering nature of naturopathic medicine. A naturopathic doctor simply provides the tools, education, and resources for each patient to work on their own healing.
- 02 Jul 14
If you are serious about athletics, or know someone who is, you already know that athletes are a slightly different breed of human. They flirt with the extreme limits of human physiology, and feed off the adrenaline it produces. Their success often hinges on the most seemingly nominal criteria: seconds, ounces, and inches.
Newsletter
Most Popular
- 07 May 15
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13