Related Articles
- 15 Sep 23
Acupuncture shows promise in reducing cancer treatment side effects in small studies. Further research with larger populations and funding could boost its role in Western cancer care. With its history, minimal side effects, and energy benefits, acupuncture may become a common recommendation for cancer recovery.
- 09 Mar 15
 Prostate cancer is the most common cancer among Canadian men (excluding nonmelanoma skin cancer), with 1 in 8 Canadian men expected to develop the disease in his lifetime, and 1 in 28 expected to die from it.[1] In Canada, the five-year survival rate for prostate cancer is 96%; however, despite this promising statistic, every day an average of 65 Canadian men will be diagnosed with prostate cancer, and 11 will die from it.
Prostate cancer is the most common cancer among Canadian men (excluding nonmelanoma skin cancer), with 1 in 8 Canadian men expected to develop the disease in his lifetime, and 1 in 28 expected to die from it.[1] In Canada, the five-year survival rate for prostate cancer is 96%; however, despite this promising statistic, every day an average of 65 Canadian men will be diagnosed with prostate cancer, and 11 will die from it. - 17 Jun 16
 The use of complementary medicine for the treatment of cancer and its side effects has skyrocketed in recent years. Complementary therapies refer to ones that are nonpharmaceutical in nature, and that have the potential to not only enhance quality of life, but also to reduce side effects of conventional therapy.
The use of complementary medicine for the treatment of cancer and its side effects has skyrocketed in recent years. Complementary therapies refer to ones that are nonpharmaceutical in nature, and that have the potential to not only enhance quality of life, but also to reduce side effects of conventional therapy. - 09 Jul 15
 W. somnifera, also known as Ashwagandha, is an important herb that has been used for over 3000 years. The important constituents of the root are steroidal alkaloids and steroidal lactones referred to as withanolides. It is used for anxiety, inflammation, Parkinson’s disease, cognitive and neurological disorders, and as a supportive adjunct for people undergoing radiation and chemotherapy.
W. somnifera, also known as Ashwagandha, is an important herb that has been used for over 3000 years. The important constituents of the root are steroidal alkaloids and steroidal lactones referred to as withanolides. It is used for anxiety, inflammation, Parkinson’s disease, cognitive and neurological disorders, and as a supportive adjunct for people undergoing radiation and chemotherapy. - 09 Mar 15
 Origanum vulgare (the scientific name of oregano) has been studied in depth due to a number of interesting and exciting potential clinical uses. There is also an ongoing interest in a number of industries to replace synthetic chemicals with natural products that have similar properties. Many bioactive compounds can be found in aromatic plants, and there are a number of different ways they can be extracted.
Origanum vulgare (the scientific name of oregano) has been studied in depth due to a number of interesting and exciting potential clinical uses. There is also an ongoing interest in a number of industries to replace synthetic chemicals with natural products that have similar properties. Many bioactive compounds can be found in aromatic plants, and there are a number of different ways they can be extracted. - 08 Jan 15
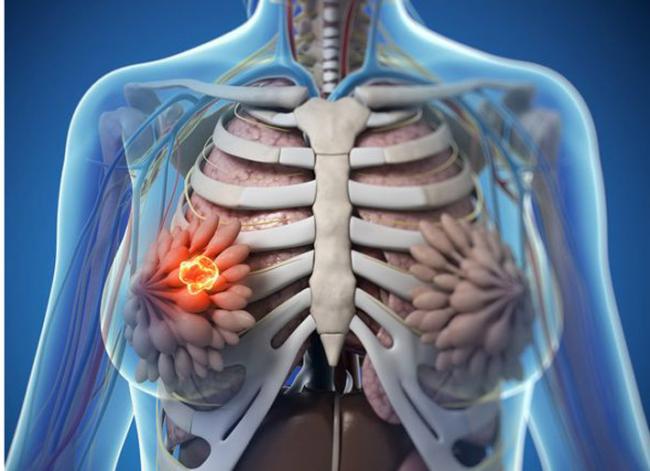
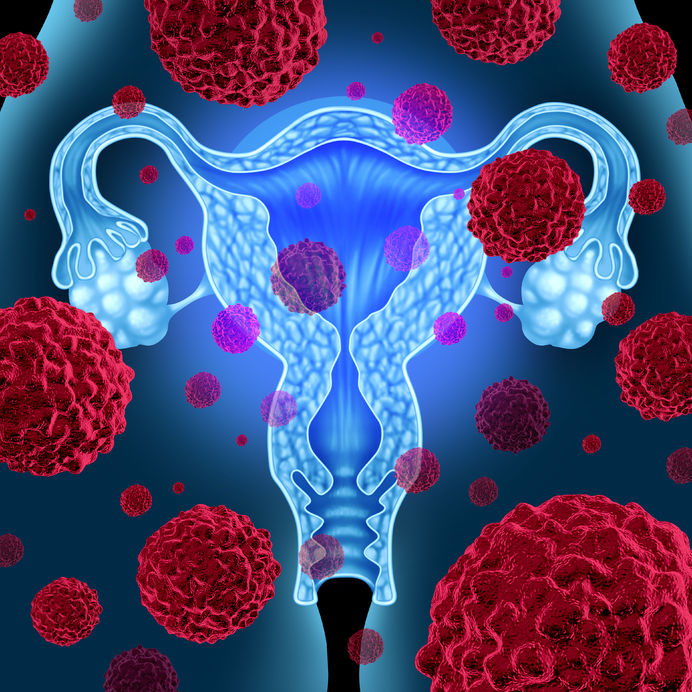 Cervical dysplasia refers to abnormal cells found on the surface of the cervix, that are considered to be premalignant and can progress to cancer.[1] Cervical dysplasia is primarily caused by a sexually transmitted infection with different strains of the human papillomavirus (HPV). However, different strains can be involved in both benign and malignant lesions; therefore, the progression of the disease appears to depend on individual factors. Studies suggest that HPV exposure is the initiating event that can lead to the development of cervical dysplasia, often termed cervical intraepithelial neoplasia (CIN).
Cervical dysplasia refers to abnormal cells found on the surface of the cervix, that are considered to be premalignant and can progress to cancer.[1] Cervical dysplasia is primarily caused by a sexually transmitted infection with different strains of the human papillomavirus (HPV). However, different strains can be involved in both benign and malignant lesions; therefore, the progression of the disease appears to depend on individual factors. Studies suggest that HPV exposure is the initiating event that can lead to the development of cervical dysplasia, often termed cervical intraepithelial neoplasia (CIN). - 03 Apr 14
 In this issue, we take on an unusual topic for a naturopathic publication: the novel, anticancer activity of a prescription medication, metformin. Metformin is best known as a diabetes medication; it commonly used as the first-line medication for type 2 diabetes, as well as conditions of prediabetes, such as polycystic ovary syndrome (PCOS). There is increasing interest in metformin in the treatment and prevention of cancer, including among naturopathic physicians specializing in oncology.
06 Sep 1616 Jan 17
In this issue, we take on an unusual topic for a naturopathic publication: the novel, anticancer activity of a prescription medication, metformin. Metformin is best known as a diabetes medication; it commonly used as the first-line medication for type 2 diabetes, as well as conditions of prediabetes, such as polycystic ovary syndrome (PCOS). There is increasing interest in metformin in the treatment and prevention of cancer, including among naturopathic physicians specializing in oncology.
06 Sep 1616 Jan 17The topic of how diet affects prostate cancer has been a topic of interest for a while. It is known that the risk of prostate cancer varies dramatically based on geographic location—in some places, the risk is 60 times higher than others!
10 Apr 1613 Oct 1503 Feb 15 Without question, receiving a cancer diagnosis is life altering, and may bring with it more fear than any other diagnosis. Patients may fear for their life, fear telling their family, friends and coworkers, and fear what the treatment will be like. This has a huge psychological impact, and stress levels are drastically increased.01 Feb 14
Without question, receiving a cancer diagnosis is life altering, and may bring with it more fear than any other diagnosis. Patients may fear for their life, fear telling their family, friends and coworkers, and fear what the treatment will be like. This has a huge psychological impact, and stress levels are drastically increased.01 Feb 14$path = isset($_GET['q']) ? $_GET['q'] : '
';
$link = url($path, array('absolute' => TRUE));$nid = arg(1);
if ($nid == 201402){
?>download pdf
}
?> Resveratrol is an important phytonutrient and antioxidant that naturally occurs in the skin of red grapes, peanuts, and some berries, and is touted as the health-promoting compound found in red wine. In the last few years, resveratrol research has exploded. Well over 1,000 research papers have been written to examine the health benefits of this plant compound in the past two years alone.
10 Apr 16
Resveratrol is an important phytonutrient and antioxidant that naturally occurs in the skin of red grapes, peanuts, and some berries, and is touted as the health-promoting compound found in red wine. In the last few years, resveratrol research has exploded. Well over 1,000 research papers have been written to examine the health benefits of this plant compound in the past two years alone.
10 Apr 16 Every woman—if she lives long enough—will experience menopause. For some, the transition is easy and can even be a relief from the troubles of a regular menstrual cycle. For others, the change is extremely challenging as they struggle to manage frequent “hot flashes,” weight gain, and severe depression. Many of the symptoms of menopause can be directly related to the decreased production of sex hormones— specifically estrogen and progesterone.17 May 18
Every woman—if she lives long enough—will experience menopause. For some, the transition is easy and can even be a relief from the troubles of a regular menstrual cycle. For others, the change is extremely challenging as they struggle to manage frequent “hot flashes,” weight gain, and severe depression. Many of the symptoms of menopause can be directly related to the decreased production of sex hormones— specifically estrogen and progesterone.17 May 18Magnesium is the fourth most-abundant mineral in the human body, and is essential for the hundreds of metabolic and hormonal reactions occurring daily. It is generally known to be a component of bone formation (partnered with calcium), and is gaining more interest as a sleep aid due to its natural muscle relaxant properties.
02 Oct 22Mushrooms are jam-packed superfoods that have been used in culinary and medicinal preparations for thousands of years. They are full of nutrients including proteins made of amino acids, fibers, carbohydrates—including polysaccharides (β‑glucans), vitamins (B2, B3, folate/B9, B12, C, D2, and E), and minerals (K, P, Mg, Ca, Cu, Fe, and Zn).
05 Jun 14
Quercetin is a member of the flavonoid family of compounds. Flavonoids, sometimes referred to as bioflavonoids, are part of what give fruits and vegetables colour. Quercetin is more specifically a flavonol, which is a subclass of flavonoids. There are many subclasses of flavonoids, and within each subclass, there are many compounds. Quercetin is just one of the compounds in the flavonol subclass. The compounds in each subclass have a similar chemical structure.07 May 15 Sunlight has been an integral part of human evolution and the development of life on this planet. Sunlight provides energy to grow plants, providing us with food, shelter and various tools. It is also essential to regulating the seasons. Thus, it has become a necessary component of life as we know it.03 Jan 14
Sunlight has been an integral part of human evolution and the development of life on this planet. Sunlight provides energy to grow plants, providing us with food, shelter and various tools. It is also essential to regulating the seasons. Thus, it has become a necessary component of life as we know it.03 Jan 14$path = isset($_GET['q']) ? $_GET['q'] : '
';
$link = url($path, array('absolute' => TRUE));$nid = arg(1);
if ($nid == 201401){
?>download pdf
}
?> Turmeric is a golden-color spice widely used in South Eastern and Middle Eastern cooking. Besides being a popular spice, it is also an important herb used in many disciplines of medicine. The medicinal use of turmeric dates back to 4000 years ago in India. It takes on many different names: Indian saffron, haldi, rhizoma curcumae (jiang huang), asterre merite.
07 Jan 22
Turmeric is a golden-color spice widely used in South Eastern and Middle Eastern cooking. Besides being a popular spice, it is also an important herb used in many disciplines of medicine. The medicinal use of turmeric dates back to 4000 years ago in India. It takes on many different names: Indian saffron, haldi, rhizoma curcumae (jiang huang), asterre merite.
07 Jan 22For centuries, mushrooms have been foraged and added to soups and stews for their robust nutritional profile. Fungi are much smarter than we think for what simple organisms they are.
Newsletter
Most Popular
- 07 May 15
- 27 Jan 21
- 03 Nov 16
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13