Diet and Osteoporosis - Naturopathic Perspectives
Bone is our main structural support system. It allows us to protect our vital organs, facilitates movement and creates a scaffold for blood vessels and nerves. In additional to the structural functions, bone has important metabolic and endocrine functions as well. Bone functions as a reservoir for minerals like calcium, phosphate and magnesium, and as such, it has the capacity to influence acid base balance, muscle contractions, neuronal communications, blood coagulation and heart rhythm. Recently, it has been discovered to be involved in the body’s stress response, and thus influence hormone functions. The relationship between bone and these various systems is bidirectional. This is of no surprise, as most of the body’s organs function in a complex way integrated into the functions of neighboring organs. In the case of bone it requires a healthy digestive system for absorption of nutrients, kidneys and parathyroid glands to regulate calcium levels, and the immune and endocrine systems, including hormones like estrogen, testosterone, insulin and growth hormone. That’s just to name a few. When one or more of these systems is strained and is unable to meet the bone’s physiological needs conditions like osteoporosis can occur.
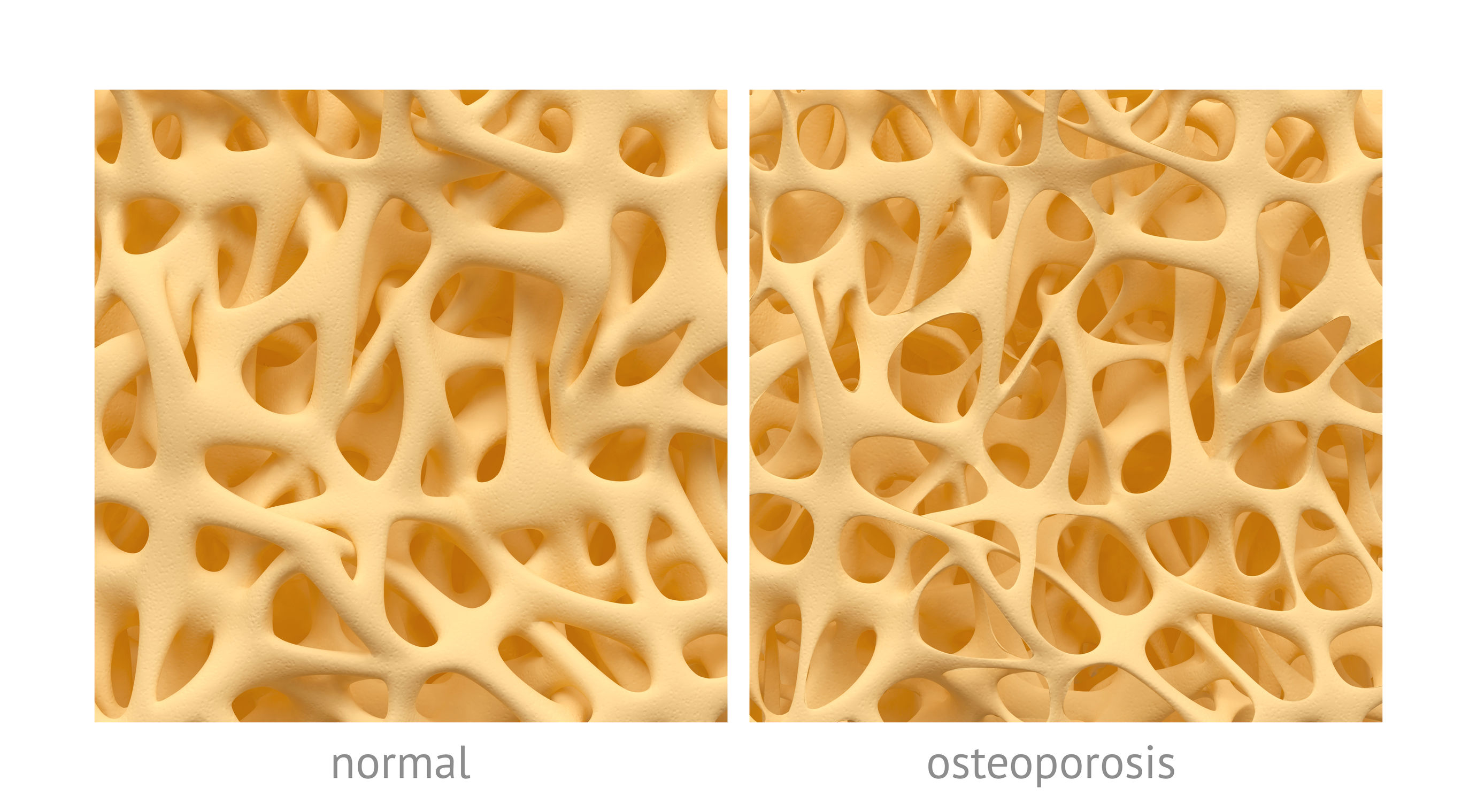
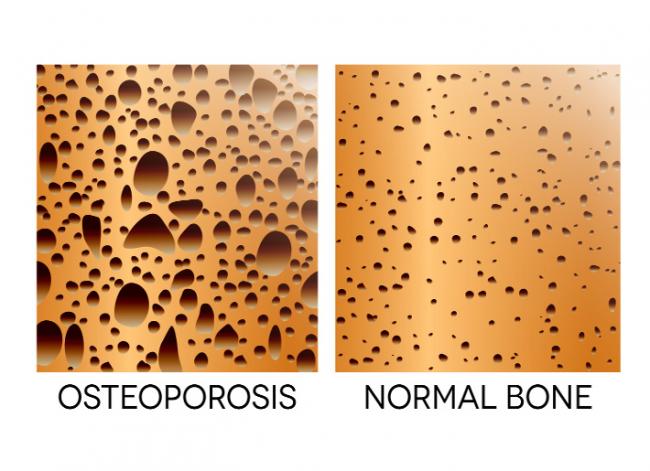
Osteoporosis affects ten percent of the Canadian population over the age of 40. In fact, one in five men and one in three women will have an osteoporotic fracture at some point in their life. As the population ages, the number of patients experiencing osteoporosis increases. Basically, osteoporosis and its impact are increasing. The nature of the condition is systemic and results in an imbalance between bone formation and bone resorption (breaking down of bone). The production cannot keep up with the destruction and the bone
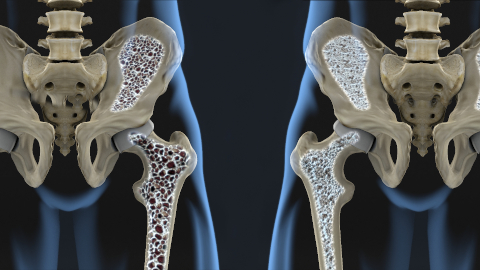
becomes weak and susceptible to fractures. When exploring the causes of osteoporosis, it quickly becomes clear that this is not simply a deficiency of calcium, vitamin K or vitamin D that is driving this beast. While the condition has a very strong genetic component (between fifty and eighty percent) it is also correlated with health and lifestyle factors such as: alcohol use, prolonged use of various medications (like corticosteroids and antidepressants), low BMI, gastrointestinal disorders, thyroid disease, eating disorders and many others. Recent research in microbiology is demonstrating a change in the gut flora in patients with osteoporosis. Thus, there may even be a microbiological cause or strong influence. Given the diversity of the systems involved, it seems reasonable to consider a holistic approach to treatment and examine the impact that diet can have on this condition.
Several nutrients have been implicated in the health of bone. These are calcium, vitamin D, vitamin K, silica, boron and iron. Numerous studies have explored the value of calcium in fracture risk prevention and compared it to that of increased heart attack risk (1). Unfortunately, with or without vitamin D, the risk benefit ratio is still unclear. Every year new meta-analyses and systematic reviews explore the clinical trials and observation research trying to uncover the answers – should we be supplementing with calcium, and if so, how much? The research on vitamin D and vitamin K suggests that they are important to bone health, but supplementation alone is not the answer to reducing fractures. More research is needed to evaluate the benefit of supplementation with individual micronutrients, like silica and boron. In terms of iron, the studies demonstrate that both a deficiency in iron and iron overload can put the bones at risk of fracture. In the case of overload, excess iron can be deposited in the bones and causes damage to osteoblasts, while the mechanism with iron deficiency is less clear (2). Thus, it is prudent to consider the value of these nutrients from a different perspective. What about whole foods? What are the foods that provide us with these and other, maybe yet to be correlated to osteoporosis, nutrients?
The calcium rich foods include the well-known dairy products, sardines and soy. The vegetarian options include almonds, white beans, molasses, figs, collard greens, broccoli, bok choy and other greens. While the dairy and fish options provide higher amount of calcium per gram, the cooked vegetables and almond flour can match these when included in a daily diet. For vitamin D there are lots of fortified options, such as cereals, orange juice and dairy. The non-fortified foods include fatty fish, like salmon, liver, eggs and surprisingly, portabella mushrooms. There are two different types of vitamin K. The vitamin K2 is correlated in observation studies to osteoporosis risk prevention, while vitamin K1 is known for its coagulation effects. This vitamin is available in fermented soy, cheese, egg yolk, grass fed beef and organ meats. With respect to the micronutrients, silica is found readily available in bananas, green beans, various vegetables, breakfast cereals and various fruits, while boron is located in leafy greens, prunes, raisings, grains, apples and beans.

Thus, it appears that the “osteoporotic diet” is closely aligned to the Mediterranean diet. Mediterranean diet recommends a hefty amount of fruits and vegetables followed by grains and cereals. Animal products like dairy, eggs, fish and chicken are advised on sporadic bases. In fact, a large systematic review of close to two hundred thousand participants demonstrates a seven percent reduction in fracture risk for those following the Mediterranean diet for an average of 9 years (3). More specifically, the risk is reduced for fractures of the hip, which are known to be associated with increased mortality within the first year. Other studies of this diet demonstrate statistically significant increase in bone mineral density and markers of osteoblast activity. Osteoblasts are the cells that produce the structural matrix of the bone.
Another way to examine the nutrients and foods that contain them is to look at the protein amounts and sources with respect to osteoporosis risk. Observation study from Korea reports that diets poor in protein, as in where protein accounts less than ten percent of the daily food intake, correlate with increased prevalence of osteoporosis, while diets rich in protein, where it accounts for more than twenty percent, appear to be protective. This observation was true for both men and women. Thus, the amount of protein appears to be important. However, another studied compared three diets, with differing amounts of protein suggests it is not the amount of protein that’s important. The first diet provided a very high amount of animal protein per day, close to two hundred grams. The second was considered a “low meat” diet, instead it provided lots of fruits and vegetables and only thirty-five grams of protein. The last diet mimicked the “low meat” but it included mineral supplementation. Of these three diets, the diet that appeared to preserve calcium was the “low meat” with mineral supplements. There was no difference between the high and low meat diets if they did not contain the mineral supplement (4). This would suggest that minerals are at least, if not more, important than the protein. However, the high protein diet of over two hundred grams of protein is not representative of the typical, healthy amount of protein. It is almost excessively high. As well, the study used urinary calcium as its outcome, which is weakly associated with osteoporosis. Thus, its results should be taken with a grain of salt.

The ketogenic has become a very fashionable diet for its success in weight loss and epilepsy. In fact, it is also being explored for Parkinson’s disease, dementia and diabetes. Ketogenic diet is focused on delivering high amounts of fat, while keeping carbohydrates to a very strict minimum. The purpose is to starve the body of carbohydrates and force it to use fats as the main source of fuel. When it comes to osteoporosis, the outcomes of this diet are rather concerning! A study with twenty-five children suffering with epilepsy where put on the ketogenic for 15 months (5). At the end of the study they were ingesting suboptimal amounts of calcium and vitamin D. What’s worse is that their bone mineral content was rapidly declining. While this is a small study of only twenty fiver participants it should raise alarm bells for anyone considering doing the ketogenic diet for a prolonged amount of time.
Osteoporosis causes significant disability and even mortality, as in the case of hip fractures, worldwide. As the population ages, this becomes a more pressing issue. While the research on nutrient supplementation is searching for the right dose and the full list of necessary nutrients, dietary research is demonstrating some protection. The Mediterranean diet provides a seven percent fracture risk reduction when followed for a prolonged amount of time (such as nine years). It is rich in calcium, vitamin D, boron, vitamin K and silica, all of which have been implicated in fracture risk prevention in some capacity. While there are interesting diets that help with weight loss, like the ketogenic diet, these may cause problems when followed long terms. This is seen with children who stayed on the diet for over a year and resulted in loss of bone mineral content. Thus when exploring a dietary approach to osteoporosis it is prudent to look beyond calcium and vitamin D and consider a wide range of nutrients and macromolecules and their impact on bone health.
References:
- Bolland M. Vascular events in healthy older women receiving calcium supplementation: randomized controlled trial. BMJ. 2008; 336(7638): 262-266
- Che J, et al. The effect of abnormal iron metabolism on osteoporosis. Biol Trace Elem Res. 2019.
- Benetou et al. Mediterranean diet and incidence of hip fracture in a European cohort. Osteoporosis Int. 2013; 24(5): 1587-98
- Massey L. Dietary animal and plant protein and human bone health: a whole foods approach. J Nutr. 2004; 134(11): 3100-3105
- Bergqvist C, et al. Progressive bone mineral content loss in children with intractable epilepsy treated with ketogenic diet. The Amer J of Clin Nutr. 2008; 88(6): 1678-1684