The Naturopathic Pillars of Treating Adult Acne
What is Acne?
Acne (or acne vulgaris) is one of the most common skin conditions, affecting 64% of people in their 20s and 43% of people in their 30s [1]. It affects the pilosebaceous units of the skin, which is essentially the oil gland and hair follicle. It usually affects the largest, hormone-responsive sebaceous glands such as those on the face, chest, neck and back. Acne lesions themselves can be either non-inflammatory (ie. blackheads and whiteheads), or inflammatory with pus-filled or deep, cystic lesions [1]. It can be graded as mild, moderate or severe depending on the presentation [2]. Mild acne is present only on the face, while moderate presentation will have more lesions with one to two cysts or nodules and may expand to other body parts. In the case of severe acne, there are usually several cystic or nodular lesions and involvement of skin other than the face. With this extent of severity, scarring of the skin is quite common [2]. There is a huge psychological component associated with acne as it can be quite troublesome and frustrating. The goal of this article is to identify the potential causes of acne and lifestyle or hormonal triggers which can exacerbate its presentation.
What Causes Acne?

The cause of acne can vary individually, which is why it is important to identify the unique cause in order to treat the source. There is often a family history associated with severe cases of acne, where an immediate family member has experienced similar severity [1]. Aside from genetic relation, the actual pathology of acne can be linked to a few causes:
- Increased androgens* causing greater oil production by the sebaceous glands, which can lead to clogging of pores and inflammation
- Increased growth and multiplication of skin cells, which can cause oil and dead skin cells to get trapped within the follicle (often turning into a whitehead or black head)
- Colonization of the follicle by Propionibacterium acnes, which is a species of bacteria that normally lives on the skin’s surface but in certain conditions can overgrow
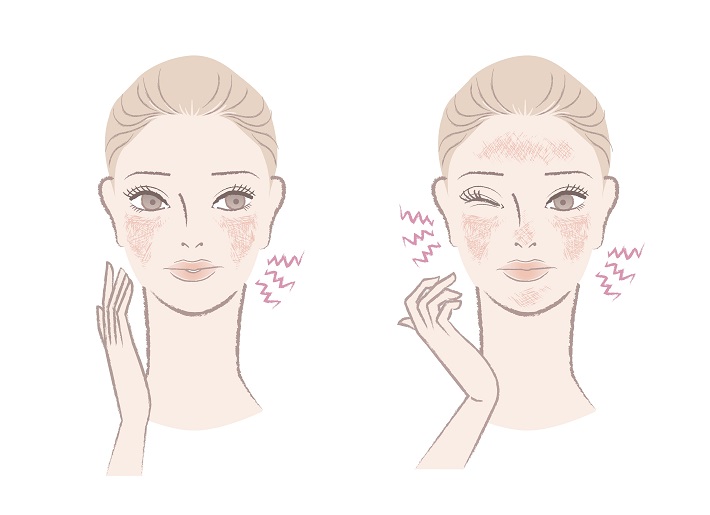
- Immune inflammatory response that is not well-understood. This can also be related to another condition called seborrheic dermatitis which is presents as red dry, flaky skin present on the scalp, eyebrows and nasal folds [3].
*Androgens are hormones that both males and females produce, although men produce them in greater quantities (ie. testosterone).
Naturopathic Pillar Treatments for Acne:
Lifestyle/Hygiene:
In general, it is best to cleanse the skin at least once to two times per day, in the morning and at night. It is also important to avoid over-washing or scrubbing the skin too hard, because this can damage the skin’s barrier, removing healthy oils from the surface which can actually trigger increased oil production [1]. For makeup users, it is imperative to thoroughly remove makeup before cleansing the skin. In terms of makeup and skincare products, the labelling should state that the product is non-comedogenic, meaning that it does not contribute to blocked pores. The skin surface is acidic in pH, so skincare products which are closer to an acidic pH (5.5-7) are more beneficial to a healthy balance of the skin’s microbiome [4]. Most soap cleansers are alkaline, so it may be helpful to look for a gentle non-soap cleanser [1]. Additionally, ensure that items which touch the face often are being cleaned on a regular basis (ie. pillowcases, phone screens).
Dietary triggers or underlying food sensitivities:
A diet rich in vitamins and nutrients is important to produce healthy skin cells. This means eating an adequate amount of food that is right for your body, activity level and health concerns. On top of this, having healthy digestive function is required to properly absorb these nutrients. Signs of poor digestive function or malabsorption include upset stomach, gas, bloating, changes in bowel movements (constipation or diarrhea), acid reflux, or food sensitivities. The difference between a food sensitivity and a food allergy is that food allergies are an Ig-E mediated reaction to certain allergens which produce symptoms such as itchy eyes, hives or even more life threatening symptoms such as difficulty breathing and throat swelling. Food sensitivities are generally Ig-G mediated and can often be subtler, such as signs of poor digestion as mentioned earlier as well as headaches or fatigue after eating and skin symptoms (ie. acne, eczema) [5]. The food sensitivities most commonly associated with acne vulgaris are dairy products, and foods with a high glycemic load [1,6].
Glycemic load is an indicator of the amount of carbohydrates in food and how quickly it will affect blood sugar levels. Foods with a higher glycemic load, such as processed foods (ie. fast food), sweetened foods, white grains and carbohydrate sources that are low in fiber, will spike blood sugar levels faster than those with a lower glycemic load. Diets which are rich in high glycemic load foods cause greater spikes in the hormone insulin and with it, insulin-like growth factor 1 (IGF-1) [6]. Insulin is responsible for responding to the increase in blood sugar by allowing cells of the body to absorb and utilize this sugar for energy. However, insulin and IGF-1 increase the production and availability of androgens in the body, which then increase oil production of the skin and the likelihood of clogged pores. Additionally, if there is an underlying food sensitivity which is being consumed in the diet, the can propagate inflammation. The role of dairy products in acne production works in a similar way by increasing insulin and IGF-1, sometimes comparable to high glycemic load foods [6,7]. Milk itself may be hormonally and biochemically active [1].
Additionally, Western diets are often higher in inflammatory omega fatty acids (omega-6), coming from highly processed foods, comparatively to omega-3s which are anti-inflammatory. In non-Western diets, the ratios of these fatty acids are balanced, whereas in Western diets, the ratio of omega-6 to omega-3 can range from 10:1 to even 20:1 [7]. This can contribute to a pro-inflammatory state which can present itself in the body, but also in the skin. For this reason, there is importance of being mindful of increasing sources of the omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) through food. Animal sources are best found in fatty fish, such as the “SMASH” fish; salmon, mackerel, anchovies, sardines and herring. Vegetarian sources of omega-3s are mainly in the form of alpha-linolenic acid (ALA), which is converted in smaller amounts to EPA and DHA which are used by the body. Highest amounts of plant-sources of omega-3s are in algae, but they can also be found in flaxseed oil, chia seeds and hemp seeds.
How to Support Healthy Digestive Function:
For support of a healthy digestive system, it is best to eat food in a relaxed environment, chewing slowly and enjoying it. This will allow the body to switch to the parasympathetic nervous system phase in order to adequately to “rest and digest”. Additionally, warm, well-cooked foods are easier to digest for individuals with sluggish digestion. It may also be important to consider foods which are high in probiotics such as kefir, sauerkraut, kimchi and kombucha, as well as foods that are high in prebiotics. Prebiotics are essentially foods which help good bacteria thrive in the digestive tract, similar to fertilizer for plants. Foods high in prebiotics are fibrous foods, garlic, onions and ground flaxseeds.
Hormonal Causes of Acne:
- Premenstrual-related cyclic acne

This type of acne refers to lesions which present around ovulation (often day 14 of the menstrual cycle) before menstrual flow begins. During this period of time, and egg is released from one of the ovaries, and levels of progesterone are slowly beginning to rise comparatively to estrogen, which contributes to the increased production of oil in the sebaceous glands. Additionally, throughout the entire menstrual cycle, androgens such as testosterone and dehydroepiandrosterone sulfate (DHEA-S) are produced in small amounts. During the peri-menstrual time, these androgens are relatively higher in ratio compared to estrogen which can result in accumulation of oil and dead skin cells in the follicle [8]. Treatment for this cause of acne could look into female hormonal balancing, or simply ensuring to decrease pro-inflammation through diet to combat and exacerbations, as these changes in hormone levels are normal.
2. Polycystic ovarian syndrome (increased androgens)
Polycystic ovarian syndrome (PCOS), is a common female hormonal condition whose cause is not quite known. It is characterized by irregular periods, especially long bouts in between periods, along with other potential symptoms of male-pattern hair growth, acne and difficulty getting pregnant [9]. The acne associated with PCOS is usually in the lower 3rd of the face, potentially on the shoulders and back and can be deep and cystic. Around 40-50% of women with PCOS are overweight, but around 50% can be normal weight as well. The treatment for this type of acne is to get to the root cause, which is androgen excess. This could include hormonal support to decrease androgens as well as a proper diet which is low glycemic loads with increased fiber and lean protein.
- Stress-related

Cortisol is a stress hormone which is released during period of mental or physical stress. Of course, stress is inevitable, and increased cortisol in the short-term is actually beneficial for short-term memory, focus and endurance. However, if an individual is unable to recognize signs of stress or adequately process them, it can lead to chronic stress and increased cortisol cycling which could negatively affect the whole body, including the skin. In response to stress, corticotropin-releasing hormone (CRH) released from the brain, travels to the adrenal glands on top of the kidneys signaling for them release cortisol. CRH itself causes increased oil production in the sebaceous glands as well as directly increasing certain inflammatory molecules (interleukin 6 and interleukin 11) which can contribute to inflammatory acne [1]. Furthermore, chronically increased cortisol can lead to insulin resistance, meaning there is more insulin and IGF-1 floating around in the bloodstream.
As was previously mentioned, the type and cause of acne varies from individual to individual, and treating various health conditions is often not a linear journey. Please speak to your healthcare practitioner before beginning a specific treatment to ensure that it is the right one for you.
References:
- Grobel H & Murphy S. 2018. Acne vulgaris and acne rosacea. Integrative Medicine 4th Edition, Elsevier Inc. Retrieved from Clinical Key.
- N.A. 2019. Clinical overview: acne vulgaris, Elsevier Point of Care. Retrieved from Clinical Key.
- Kim G. 2009. Seborrheic dermatitis and Malassezia species, Journal of Clinical and Aesthetic Dermatology. 2(11):14-17. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2923939/
- Korting HC, Hubner K, Greiner K, Hamm G & Braun-Falco O. 1989. Differences in skin surface pH and bacterial microflora due to the long-term application of synthetic detergent preparations of pH 5.5 and pH 7.0. Results of a crossover trial in health volunteers, Acta Dermato-venereologica. 70(5):429-431. Retrieved from https://europepmc.org/article/med/1980979
- Atkinson W, Sheldon TA, Shaath N & Whorewell PJ. 2004. Food elimination based on IgG antibodies in irritable bowel syndrome: a randomized controlled trial, Gut. 53(10): 1391-1393. Retrieved from https://gut.bmj.com/content/53/10/1459.short
- Melnik B & Schmitz G. 2009. Role of insulin, insulin-like growth factor-1, hyperglycaemic food and milk consumption in the pathogenesis of acne vulgaris, Experimental Dematology. 18(10). Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1111/j.1600-0625.2009.00924.x
- Pappas A. 2009. The relationship of diet and acne, The Journal of Dermato-Endocrinology. 1(5): 262-267. Retrieved from https://www.tandfonline.com/doi/full/10.4161/derm.1.5.10192
- Geller L, Rosen J, Frankel A & Goldenberg G. 2014. Perimenstrual flare of adult acne, The Journal of Clinical and Aesthetic Dermatology. 7(8):30-34. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4142818/
- N.A. 2019. Clinical overview: polycystic ovarian syndrome, Elseiver Point of Care. Retrieved from Clinical Key.