Eating Fat Isn’t the Only Thing Causing Fatty Liver Disease
In many countries around the world, alcoholic beverages are built into the culture and religion. We consume it as a form of celebration and a form of self-medication. But over the years, it takes a toll on our organ system that works to filter it out. Fatty liver disease is a growing concern in the Western hemisphere, especially as new diagnoses include people of normal body weights and people who don’t drink alcohol.
HOW FAT GETS STORED

Too much of anything is not good for the human body. In ancestral times, the human body adapted to feast or famine. When there was food to eat, our metabolisms increased and we stored food to get us to the next meal. That next meal could have been days away, which means that storage was useful. Today, food is readily available to us. We can eat when we want, as much as we want and whatever we want. However, because our physical activity has decreased (we no longer have to go out and hunt for our meals), the calories we consume that are not immediately needed are stored for later. Our next meal comes when we haven’t emptied our storage, and more and more gets stored. The most common form of storage in the human body is fat. Fat holds a large number of calories per unit, which makes it an essential fuel to prevent starvation. The liver is the organ responsible for filtering fat out of the blood. When the amount to be filtered outweighs the liver’s ability to clear it, fat begins clogging up the liver.
WHAT BECOMES FAT
When I ask my patients where they think a fatty liver comes from, the answer is always some variation of “fried foods”. Yes, fried foods, alcohol, oily and greasy foods will all increased cholesterol and the risk of a fatty liver. However, since fat is a storage form of anything in excess, too much bread, sugar, carb, juice, etc. can all contribute to fatty liver as well. You’ll note that none of these foods are greasy or fried, so understanding how this may result in fatty liver is often difficult for people.
WHEN FATTY LIVER BECOMES A PROBLEM
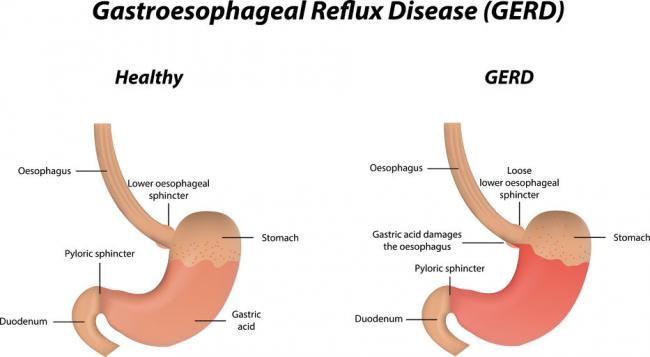
When more than 5% of the liver becomes saturated with fat, it is deemed to be a fatty liver (1). This does not cause immediate harm, but does reduce the liver’s ability to continue its regular activities, which include detoxification. If the liver cannot detoxify the body as easily, medications and waste will not be eliminated from the blood as easily. This puts the entire body at risk of toxicity. Over time, a fatty liver causes inflammation and can lead to scarring and permanent liver damage. This can also increase the risk of liver disease and liver cancers.
CO-MORBIDITIES TO FATTY LIVER
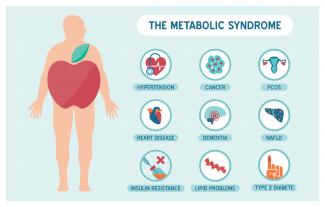
The most common cause of fatty liver disease in Canada is obesity. We know that obesity is on the rise and this makes the risk of fatty liver disease even higher in this country. New statistics show than 10% of Canadian children are obese, and that many of them are already showing signs of fatty liver disease (1). This is a disheartening statistic, especially because obesity is a completely preventable lifestyle-related disease.
Aside from obesity, it is also paired with high cholesterol, diabetes, insulin resistance and high blood pressure. These are also lifestyle-related diseases and are also on the rise in North America. Very few people have a genetic link to fatty liver disease and high cholesterol but they do exist. Certain forms of familial hypercholesterolemia or genetic variants overproduce cholesterol or have an inability to breakdown fats. These rare cases are often diagnosed early in life and can be monitored closely.
A discussion of fatty liver disease would not be complete without a discussion on medication. The most commonly prescribed pharmaceutical medication is for cholesterol-lowering, which means it targets the liver (2). Thousands of Canadians rely on multiple prescription medications every day. Thousands of other Canadians dabble in recreational drug use with or without other medications and alcohol use. Every single one of these drugs is being processed through the liver and taxing the liver’s ability to keep the bloodstream clean. Over time, there is no doubt that these medications take a toll on the liver and can lead to downstream effects.
LONG-TERM FATTY LIVER
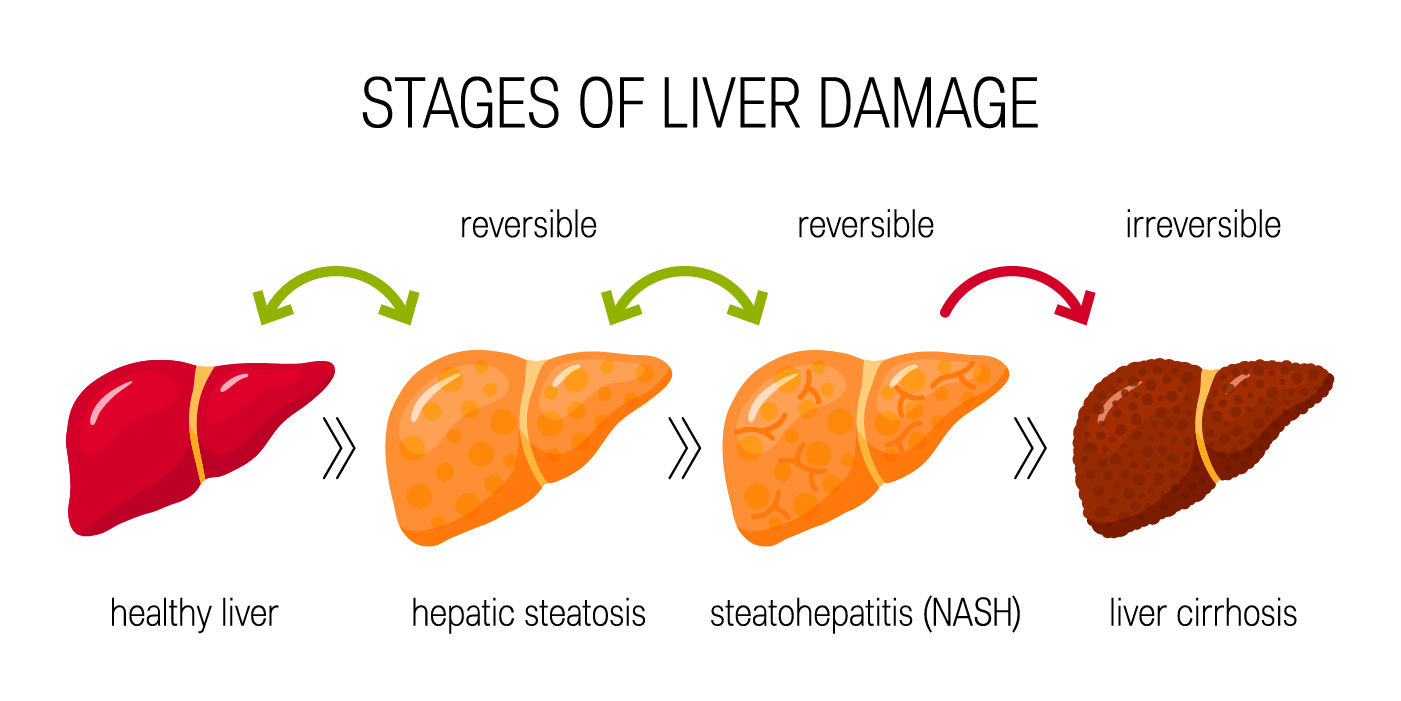 The liver does have an ability to partially regenerate, but this depends on the degree of liver damage that exists. Sometimes the damage far exceeds the body’s ability to repair it. Non-alcoholic fatty liver disease (NAFLD) is the common term used to describe a lifestyle-related fatty liver. When NAFLD becomes more extreme, highly inflamed and creates scarring, it is referred to as Non-Alcoholic Steatohepatitis (NASH). At this stage, the amount of liver damage is so extreme that many require a liver transplant due to chronic liver failure. A percentage of these will die of liver-related causes.
The liver does have an ability to partially regenerate, but this depends on the degree of liver damage that exists. Sometimes the damage far exceeds the body’s ability to repair it. Non-alcoholic fatty liver disease (NAFLD) is the common term used to describe a lifestyle-related fatty liver. When NAFLD becomes more extreme, highly inflamed and creates scarring, it is referred to as Non-Alcoholic Steatohepatitis (NASH). At this stage, the amount of liver damage is so extreme that many require a liver transplant due to chronic liver failure. A percentage of these will die of liver-related causes.
HOW TO PREVENT OR MANAGE FATTY LIVER
The good news is that reducing fat build up in the liver is entirely possible. The bad news is that there is no medication available for this, and the amount of lifestyle changes required is not easy. Management begins with a strict change in diet and lifestyle. Of course the fried, fatty foods and alcoholic beverages need to go. By reducing the amount of incoming unhealthy fat, we help to reduce the burden on the liver. By increasing the number of good healthy fats, we encourage the liver and gallbladder to work harmoniously and get rid of excessive bad fats. Similarly, the sugar consumption and high refined-carb consumption must drastically decrease. This change alone will see improvements in weight, liver and blood sugar levels within 3-5 months. While weight loss is essential, it isn’t the goal of treatment. Energy levels and sleep quality improve as whole-body inflammation decreases. An exercise routine will accelerate the rate at which improvements are seen and is a fantastic way to encourage more detoxification through the skin.
To help support your body through the changes, natural liver supports are always recommended. Some of the best liver herbs are available in tea, tincture or capsule form, which makes it much easier to reach a therapeutic dose.

- Silymarin (Milk Thistle): Unique to many herbs, this one has a lot of research to backup its effectiveness on the liver. Milk thistle has tremendous impacts on liver regeneration and has been studied for management of hepatitis, cirrhosis, NAFLD and alcoholic fatty liver disease (3).
- Burdock: This herb is often known as a ‘blood cleanser’ because of its work on the liver and supporting the filtration of waste out of the blood. It works best in combination with other liver herbs.
- Schisandra: The main target of this herb is the adrenal glands, but it also has a unique impact on the liver. Schisandra is often used preventatively for liver cirrhosis and fatty liver disease. Again, not ideal to use alone, but can be a fantastic addition to other liver supports.
- Dandelion: One of the most commonly used herbs to consume as a tea or as a leafy green vegetable. Dandelion leaf stimulates the kidneys and the root stimulates the liver. Together, this is a great whole-body detoxification support. This one may not work as strongly once you’ve already been diagnosed with fatty liver, but is a great way to prevent fat build up and encourage regular liver detox. For anyone with a family history of fatty liver or high cholesterol, adding this in regularly could be helpful.
- Turmeric: Naturopathic Doctors could write books on the effectiveness of this single herb. It is a yellow root with a powerful flavour and a wide range of effects. Turmeric is an antioxidant, anti-cancer, and anti-inflammatory herb. It affects the entire body, but because it is so bitter, its primary target is the liver. In many cultures, it is an essential part of the cuisine, but not nearly enough to see its benefits. Today, capsules are very easy to find and are likely best way to reach the therapeutic dose.
Though our liver’s have this incredible ability to repair and partially regenerate, taking advantage of this fact doesn’t help reduce our risk for other chronic diseases. Just because we can’t see or always feel the effects of a fatty liver, doesn’t mean we don’t have to do anything about it. The liver has links to skin, eyes, gut and much more. If the liver is diseased, it becomes obvious that skin tone changes, eyes become yellow and stool quality changes. At this point, the change is difficult but necessary. Getting started on supporting your liver health today can reduce the burden years down the road, and in this case, every little bit counts.
References:
- Canadian Liver Foundation (2017). Fatty liver disease. Retrieved from: https://www.liver.ca/patients-caregivers/liver-diseases/fatty-liver-disease/
- Canadian Institute for Health Information (2020). 1 in 4 Canadian seniors prescribed 10 or more drugs. Retrieved from: https://www.cihi.ca/en/1-in-4-canadian-seniors-prescribed-10-or-more-drugs
- Mulrow, C. et al. (2000) Milk Thistle: Effects on Liver Disease and Cirrhosis and Clinical Adverse Effects: Summary. AHRQ Evidence Report Summaries. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK11896/