Related Articles
- 16 Dec 19
In many parts of the world, attention deficit hyperactivity disorder (ADHD) is not a common diagnosis. But in North America, a large portion of the pediatric population is being screened and diagnosed with ADHD every day. While there are differences in culture and diet, could there be more that we are missing in our understanding of this developmental condition?
- 10 Jun 20
Growing up with both parents in the teaching profession, over the years, I’ve grown accustomed to hearing commentary on “kids these days.” Lately, the conversation seems to centre around “anxious kids” or childhood anxiety. Not only do my parents see this in schools, but I hear about it all the time in my naturopathic practice from parents and even children themselves. The stats also seem to be in agreement.
- 09 Mar 20
The link between sleep and mental health has been seen and studied for decades by doctors and researchers. People who don’t get their regular 7–9 hours of sleep per night are at 10× greater risk of depression and 17× greater risk of anxiety. To go one step further, the more frequently one wakes in the night due to insomnia, the higher the chances of developing depression.[1] Before considering pharmaceutical sleeping aids, it is important that we consider all aspects of health that can be contributing to a sleep disorder.
- 13 Feb 16
 The human microbiome is defined as the full collection of genes of all the microbes in the human body and “consists of 10–100 trillion symbiotic microbial cells,” outnumbering the number of human cells by ten times. An individual’s genome is 99.9% identical to another human’s; however, their microbiomes will only show 10–20% similarity to one another.
The human microbiome is defined as the full collection of genes of all the microbes in the human body and “consists of 10–100 trillion symbiotic microbial cells,” outnumbering the number of human cells by ten times. An individual’s genome is 99.9% identical to another human’s; however, their microbiomes will only show 10–20% similarity to one another. - 17 Jun 16
 It is clear that everyday stress in the 21st-century Western world is high. As adults, we often think of “stress” as a reaction to a traumatic event such as losing a loved one or being fired from a job, as well as from the pressures of everyday life including meeting deadlines in a high-paced work environment, personal relationship difficulties, and the all too common “glorification of busy.”
It is clear that everyday stress in the 21st-century Western world is high. As adults, we often think of “stress” as a reaction to a traumatic event such as losing a loved one or being fired from a job, as well as from the pressures of everyday life including meeting deadlines in a high-paced work environment, personal relationship difficulties, and the all too common “glorification of busy.” - 20 Feb 18
Sleep problems are very common in children. Those between the ages of 2-8 years-old often exhibit snoring or breathing difficulties, which can be a sign of obstructive sleep apnea (OSA). The main reason for this is due to the size of the adenoids and/or tonsils relative to the diameter of the upper airway at this point of physical development. The consequences of this go beyond being a “noisy” sleeper as apnea ....
- 06 Nov 14
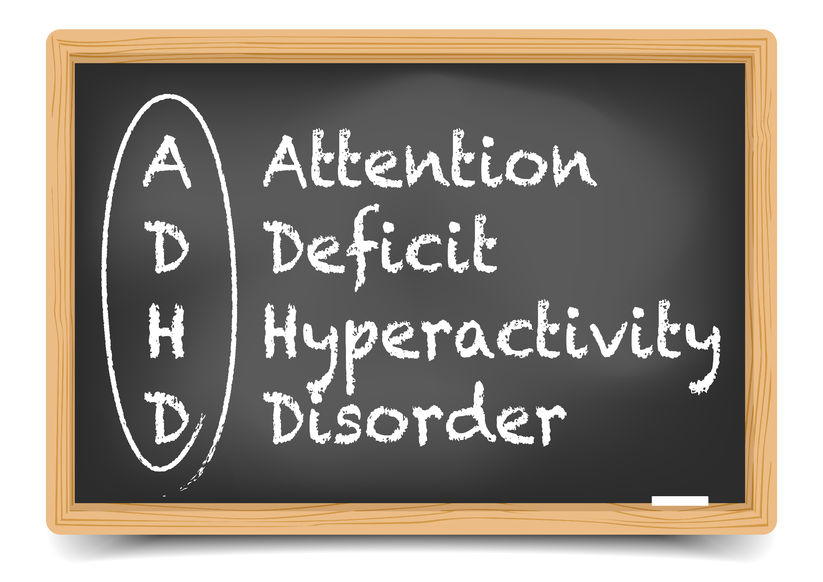
 Attention Deficit Hyperactivity Disorder (ADHD) is a common neurological concern. The estimated prevalence in children is approximately 5.29% worldwide. A Dutch study found that 70% of these children may continue to be affected as adults.[2] Some features of ADHD include: increased inattention, impulsivity, and hyperactivity.
Attention Deficit Hyperactivity Disorder (ADHD) is a common neurological concern. The estimated prevalence in children is approximately 5.29% worldwide. A Dutch study found that 70% of these children may continue to be affected as adults.[2] Some features of ADHD include: increased inattention, impulsivity, and hyperactivity. - 03 Dec 14
 Autism is a neurodevelopmental and biologically based disorder that falls within the category of pervasive developmental disorders.[1] Some consider it to be the most severe type of spectrum disorder.[2] Autism spectrum disorders include autism, Asperger syndrome, pervasive developmental disorder (not otherwise specified), childhood disintegrative disorder, and Rett syndrome.
Autism is a neurodevelopmental and biologically based disorder that falls within the category of pervasive developmental disorders.[1] Some consider it to be the most severe type of spectrum disorder.[2] Autism spectrum disorders include autism, Asperger syndrome, pervasive developmental disorder (not otherwise specified), childhood disintegrative disorder, and Rett syndrome. - 08 Jun 15
 Probiotics are a popular intervention used by naturopathic doctors in the treatment of these atopic conditions, such as eczema, allergies, and asthma, as well as digestive disorders; in fact, epidemiological evidence has shown children with atopic diseases have different intestinal (probiotic) flora compared to healthy children.
Probiotics are a popular intervention used by naturopathic doctors in the treatment of these atopic conditions, such as eczema, allergies, and asthma, as well as digestive disorders; in fact, epidemiological evidence has shown children with atopic diseases have different intestinal (probiotic) flora compared to healthy children. - 25 May 16
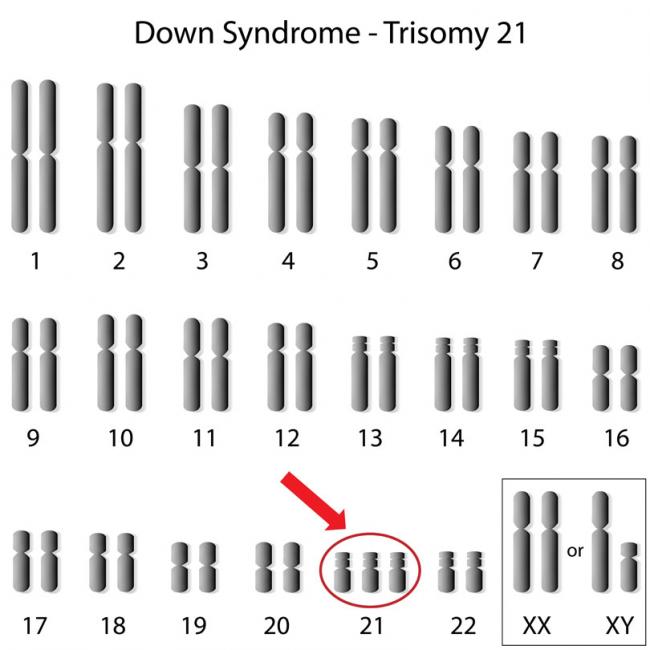
Down syndrome received its name in 1866, when John Langdon Down initially described this disorder. Down syndrome is more recently known as trisomy 21 (T21), which better describes the extra 21st chromosome that is distinctive for 95% of individuals with this genetic disorder.
- 22 Jan 18
Juvenile idiopathic arthritis (JIA) can be a painful condition for children and parents alike, as they juggle the everyday struggle while hoping for answers from the medical community. JIA is the most common childhood rheumatic illness, and is defined as a group of chronic arthritic diseases which normally occur in children under the age of 16. JIA can present with morning stiffness, swelling, and tender joints, which force many children to opt out of extracurricular activities and can leave them unable to....
- 26 Aug 13
An emerging area of study is dedicated to studying the impact of early life factors including nutrition on the development of disease later on in life. The fetal origins of adult disease (FOAD) are a field devoted to investigating the link between maternal/fetal conditions during prenatal life, and chronic disease risk in adult life. Although this makes intuitive sense, the extent of its influence was not realized until relatively recently.
- 01 Oct 13
$path = isset($_GET['q']) ? $_GET['q'] : '
';
$link = url($path, array('absolute' => TRUE));$nid = arg(1);
if ($nid == 201310){
?>download pdf
}
?>
While becoming pregnant is wonderful news, especially for couples who have faced fertility challenges, it is only the beginning of the journey. Unfortunately not all pregnancies are 40 weeks of smooth sailing. Some women are faced with more serious concerns such as vaginal bleeding (and therefore presumed threatened miscarriages) giving rise to much stress and anxiety, while others suffer from severe nausea/vomiting.
Newsletter
Most Popular
- 09 Jul 15
- 13 Feb 16
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13