Related Articles
- 28 Jan 21Advanced glycation end-products (AGEs) are compounds that are generated under hyperglycemic conditions. They could be formed endogenously, or they could be consumed from our diet. Increased presence of AGEs in the human body is associated with diverse age-related and chronic conditions...
- 12 Feb 20
Mild traumatic brain injuries (mTBIs) and postconcussion syndrome are becoming more of a public health concern. Although termed “mild,” the effects can certainly be debilitating and severe in some cases. The symptoms of postconcussion syndrome include headaches, memory and concentration difficulties, irritability, fatigue, nausea, visual disturbances, light and noise sensitivity, judgement problems, depression, and anxiety.
- 13 Apr 20
How to grow neurons—yes, you read that right!
There is a protein produced and used in our nervous system that helps the neurons grow in our brain, and which helps our brains work better, faster, stronger. In this article, we talk about things we can do to help increase the levels of this protein, and the research behind it. - 03 Dec 14
 Our society is always looking for the weight management silver bullet; that magic diet, pill, or fitness machine that will shed excess fat and lead to a fit and firm body. Over the years, a multitude of services and products have hit this multi-billion dollar industry, yet we continue to see obesity rates rise, along with its associated co-morbidities. When it comes to weight management, focusing on the fundamental constituents of healthy living, rather than fads and gimmicks, is always the best bet. However, these common approaches do not always lead to the attainment of desired results.
Our society is always looking for the weight management silver bullet; that magic diet, pill, or fitness machine that will shed excess fat and lead to a fit and firm body. Over the years, a multitude of services and products have hit this multi-billion dollar industry, yet we continue to see obesity rates rise, along with its associated co-morbidities. When it comes to weight management, focusing on the fundamental constituents of healthy living, rather than fads and gimmicks, is always the best bet. However, these common approaches do not always lead to the attainment of desired results. - 02 Jul 14
If you are serious about athletics, or know someone who is, you already know that athletes are a slightly different breed of human. They flirt with the extreme limits of human physiology, and feed off the adrenaline it produces. Their success often hinges on the most seemingly nominal criteria: seconds, ounces, and inches.
- 09 Mar 15
 Prostate cancer is the most common cancer among Canadian men (excluding nonmelanoma skin cancer), with 1 in 8 Canadian men expected to develop the disease in his lifetime, and 1 in 28 expected to die from it.[1] In Canada, the five-year survival rate for prostate cancer is 96%; however, despite this promising statistic, every day an average of 65 Canadian men will be diagnosed with prostate cancer, and 11 will die from it.
Prostate cancer is the most common cancer among Canadian men (excluding nonmelanoma skin cancer), with 1 in 8 Canadian men expected to develop the disease in his lifetime, and 1 in 28 expected to die from it.[1] In Canada, the five-year survival rate for prostate cancer is 96%; however, despite this promising statistic, every day an average of 65 Canadian men will be diagnosed with prostate cancer, and 11 will die from it. - 17 Jul 16
- 17 Jun 16
 Are you spending enough time outdoors? A recent study found that gardening can be a promising strategy to improve fruit and vegetable consumption, physical activity, and physical function in cancer survivors.[1] When we think about all of the different health habits that could have high return on investment, fruit and vegetable consumption and physical activity are at the top of the list.
Are you spending enough time outdoors? A recent study found that gardening can be a promising strategy to improve fruit and vegetable consumption, physical activity, and physical function in cancer survivors.[1] When we think about all of the different health habits that could have high return on investment, fruit and vegetable consumption and physical activity are at the top of the list. - 03 May 17
 Back pain is extremely common and has been experienced by almost everyone at one point in life. The official name for low back pain is lumbago, and it is literally defined as pain in the lower back. There are many possible causes for back pain, and often it is not even possible to identify a specific cause. If this is the case, it might be called nonspecific.
Back pain is extremely common and has been experienced by almost everyone at one point in life. The official name for low back pain is lumbago, and it is literally defined as pain in the lower back. There are many possible causes for back pain, and often it is not even possible to identify a specific cause. If this is the case, it might be called nonspecific. - 02 Sep 15
- 09 Nov 15
- 03 Feb 15
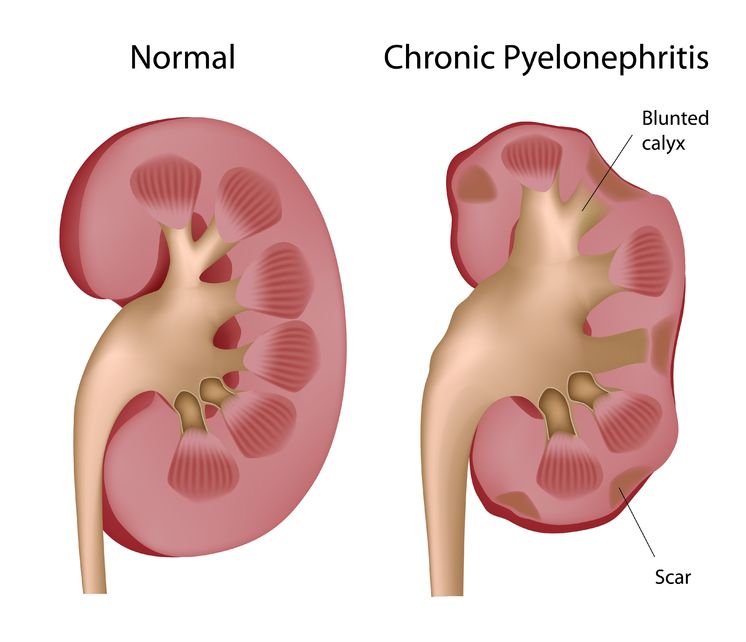
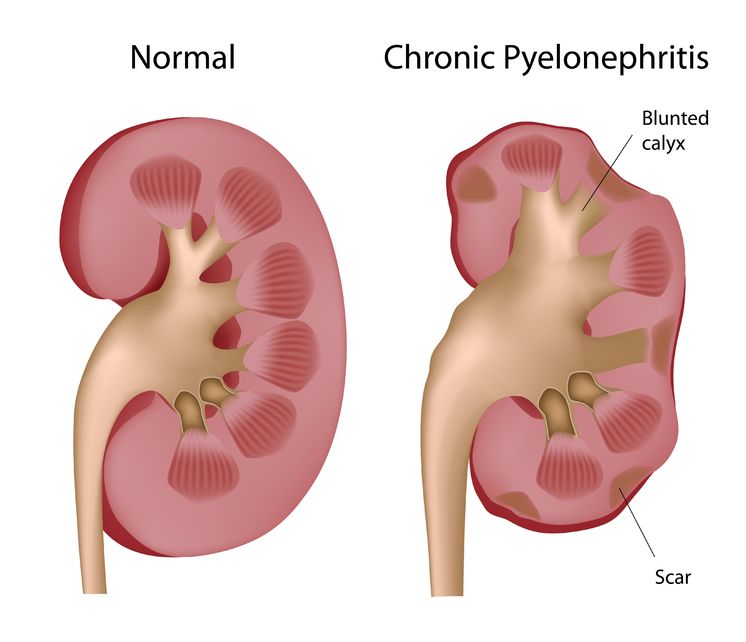 Pyelonephritis is the result of a progressive urinary tract infection, when a lower urinary infection travels upward into the upper urinary system. The lower urinary infections originate in the bladder and urethra, while the upper urinary infections involve the ureters and the kidneys. The kidneys filter the blood, so pyelonephritis can be potentially dangerous because an infection could then spread into the bloodstream.
Pyelonephritis is the result of a progressive urinary tract infection, when a lower urinary infection travels upward into the upper urinary system. The lower urinary infections originate in the bladder and urethra, while the upper urinary infections involve the ureters and the kidneys. The kidneys filter the blood, so pyelonephritis can be potentially dangerous because an infection could then spread into the bloodstream. - 09 Jul 15
 Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank.
Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank. - 02 Aug 19
Something everyone has in common is the need for sleep. We spend about one-third of our lives sleeping. Since we all need sleep, we all have different strategies and techniques in order to ensure a restful night’s sleep. Sleep hygiene are the habits one does in order to try to sleep well on a consistent basis.
- 11 Mar 16
- 18 Jan 19
A large portion of people who see naturopathic doctors come with a chief concern of digestive issues. After months of scopes and bloodwork, they are often left without answers from their medical doctor and seek a new perspective. Other times, their diagnostic imaging tests reveal something significant, yet the medical system is still at a loss for treatment options.
- 17 Aug 16
Chronic fatigue syndrome (CFS) is a chronic condition that can be difficult to diagnose and treat. It is a condition where extreme fatigue cannot be explained by any medical condition. It can get worse with mental or physical activity, but does not usually get better with rest...
- 14 Nov 19
College; it’s sometimes called “the best time in your life.” You have new people, new situations, a huge variety of extracurricular activities to choose from, all while learning about yourself and the world… It is a time full of potential!
- 09 Nov 17
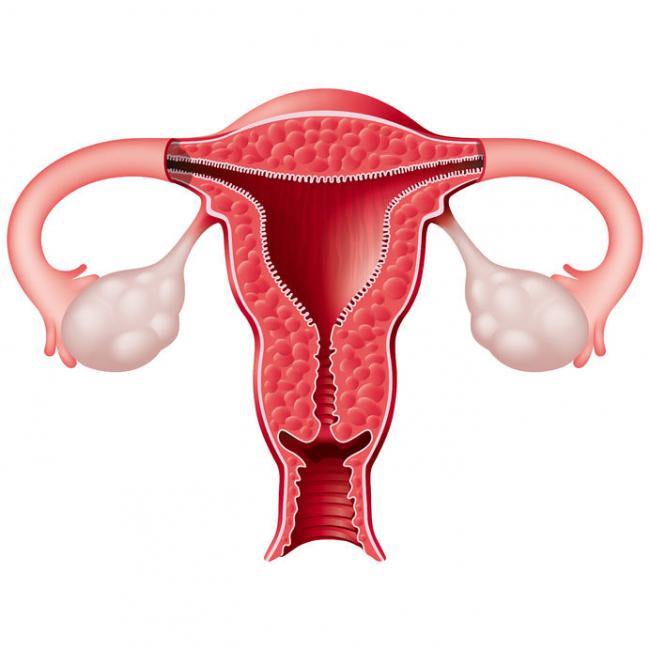
 Most women are very familiar with premenstrual syndrome (PMS), though how each individual woman experiences PMS can vary completely. Rapid fluctuations in sex hormones can lead to changes in energy, mood, and/or physical symptoms throughout her cycle, most predominantly during the last week of the luteal phase.
Most women are very familiar with premenstrual syndrome (PMS), though how each individual woman experiences PMS can vary completely. Rapid fluctuations in sex hormones can lead to changes in energy, mood, and/or physical symptoms throughout her cycle, most predominantly during the last week of the luteal phase. - 15 Sep 17
Newsletter
Most Popular
- 27 Jan 21
- 06 Oct 16
- 08 Jan 15
- 16 Jan 16
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13