Premenstrual Syndrome Factors that Cause and Aggravate PMS
desouzanaturopathic.com
Hormones are essential signaling molecules in the body, but can create extreme pain and discomfort for women if they are out of balance. Premenstrual syndrome (PMS) has been the brunt of many jokes over many decades. However, the truth of this syndrome can be devastating for the sufferer, her relationships and her career. The symptoms of PMS affect between 50 and 70 percent of all women (1). It is a major cause of absenteeism in the workplace and can manifest with a wide range of different symptoms. Many pre-existing conditions and factors go into the development of PMS that are often overlooked by medical doctors. This is because PMS is so common that women think it is normal. PMS is not normal.
PMS SYMPTOMS
An entire book could could written about the different symptoms associated with PMS, because they are different for every woman. Symptoms can range from altered libido and uterine cramps, to bloating, constipation and diarrhea. Most commonly, symptoms include backaches, water retention, swollen and tender breasts, extreme fatigue and insomnia. Many women report skin breakouts and acne in the days leading up to their period, which often disappear when it begins.
A hallmark of PMS has always been mood swings. The moodiness, anxiety, irritability and depression have consistently been associated with PMS, as well as the difficulty to control these moods and angry outbursts. When the mood symptoms become extreme, it is often termed Premenstrual Dysphoric Disorder (PMDD) (2).

CAUSES OF PMS
PMS is often linked to poor diet, high stress, and lack of exercise resulting in a hormone imbalance in the body. Quite frequently, an excess amount of estrogen in the body or an insufficient amount of progesterone will result in these symptoms. This can be aggravated by improper digestion, thyroid imbalances, and insufficient nutrients.
IMPROPER DIGESTION
In Traditional Chinese Medicine, the liver is the organ largely responsible for PMS and the menstrual cycle. It controls the movement of blood and is responsible for the feelings of frustration and irritability. In Western medicine, the liver detoxifies the blood and clears out excess hormones and waste products. If PMS has been linked to an excess of estrogen, the liver’s health should be investigated and some support for liver congestion must be included.
Similarly in the gastrointestinal tract, the bowel can often become congested and lead to an overload of waste and excess hormones. Because hormones are fat-soluble molecules, they need to be excreted in the fat-processing way, which is through the bowels. If the stomach and small intestine are improperly digesting food, there is a little more strain on the bowel to resorb as much water as possible and eliminate waste. Before we can move on to what causes an imbalance of these hormones, we must make sure our pathway of elimination are open and clear.
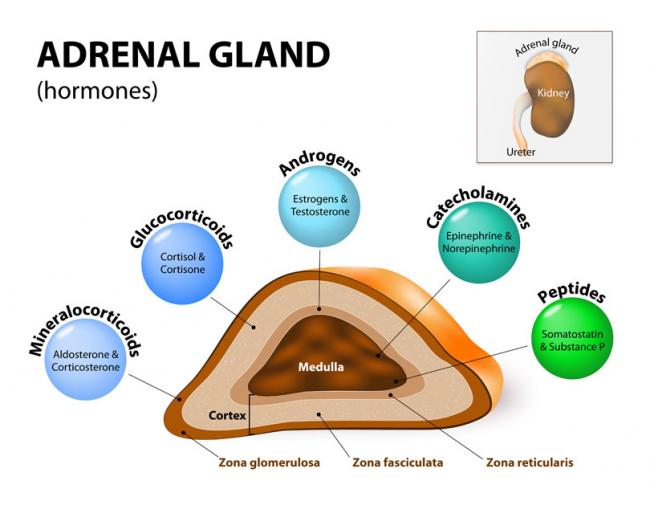
THYROID IMBALANCES
All the major endocrine glands are connected through the hypothalamic and pituitary axis. The thyroid, adrenals and ovaries are included. When there is an imbalance in one area of the body, another organ will work harder or take a hit in order to supply nutrients where it is most needed. This is an amazing and yet frustrating aspect of homeostasis. In the short term, the body can compensate for an imbalance, but in the long run, it will start to drain the resources of another organ and cause a much more complex health concern. Eventually it becomes difficult to tell where the problem began.
Thyroid imbalances are common among women and are always linked to changes in body temperature, metabolism and mood. A hypothyroid picture is often seen as weight gain, cold temperature and low mood, while a hyperthyroid picture is depicted as weight loss, increased body temperature and higher anxiety. Regardless of hyper or hypo thyroid, an imbalance in thyroid hormone is strongly associated with PMS, ovarian cysts, heavy menstrual bleeding and very painful cramping (3).
INSUFFICIENT NUTRIENTS
There are a large number of nutrients and supplements a woman could consider if suffering from PMS. Many of them can help to reduce the symptoms of PMS, but very few are responsible for causing it in the first place. Deficiencies in magnesium, vitamin B6 and iron can be strong factors in PMS. Women with PMS tend to have diets higher in refined sugars and carbohydrates, which are often not places you would find these essential nutrients.
While vitamin B6 and Magnesium help reduce PMS symptoms, iron is one that is crucial for establishing a healthy menstrual cycle. Anemia is the term to describe a low number of red blood cells in the body. Because red blood cells carry oxygen around the body, anemia limits the amount of oxygen available to the muscles, organs and tissues downstream.
Iron-deficiency is the most common form of anemia. For women, this form of anemia is likely because of the blood loss during the monthly cycle, but also the lower amount of iron they consume in their diets. Over 57% of women do not get adequate iron in their diets. The requirement is 20mg of iron daily, but most receive less than 10mg from food (4). This requirement changes during pregnancy or with factors including age, exercise intensity and dietary restriction (vegan or vegetarian).
Women who take iron supplements and still test low in iron should investigate their nutrient absorption. Iron is not an easy nutrient on the gastrointestinal tract and should really only be consumed in supplement form if someone is deficient. This goes back to the point made above that improper digestion can result in insufficient nutrients that lead to the development of PMS.
PMS is rarely the only factor causing discomfort for a woman during her menstrual cycle. Pre-existing conditions or related conditions can cause increased pain in the days leading up to the cycle, but also around ovulation.
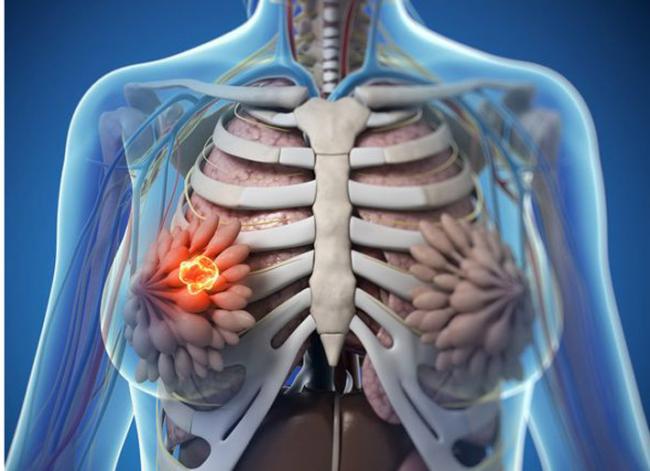
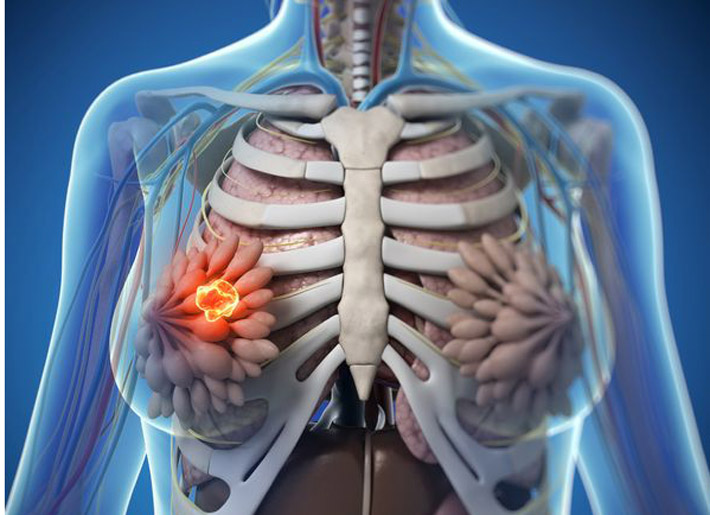
FIBROCYSTIC BREAST DISEASE
Fibrocystic Breast Disease (FBD) is a non-cancerous condition of breast tissue in which lymphatic fluid becomes trapped in small spaces and becomes encapsulated. This produces small lumps in breast tissue that do not change in size or shape and can exist for many years. These cysts may swell before and during menstruation causing pain that can range from mild to severe. Because they are affected by the rise and fall of female hormones, they generally start to disappear after menopause.

Similarly to PMS, fibrocystic breasts are linked to an excess of estrogen or low progesterone. This imbalance in the estrogen to progesterone ratio can be due to high stress, estrogen replacement therapy or overconsumption of estrogens in diet. While FBD develops outside of the menstrual cycle, because of its timing in causing pain, it is often considered a PMS symptom.
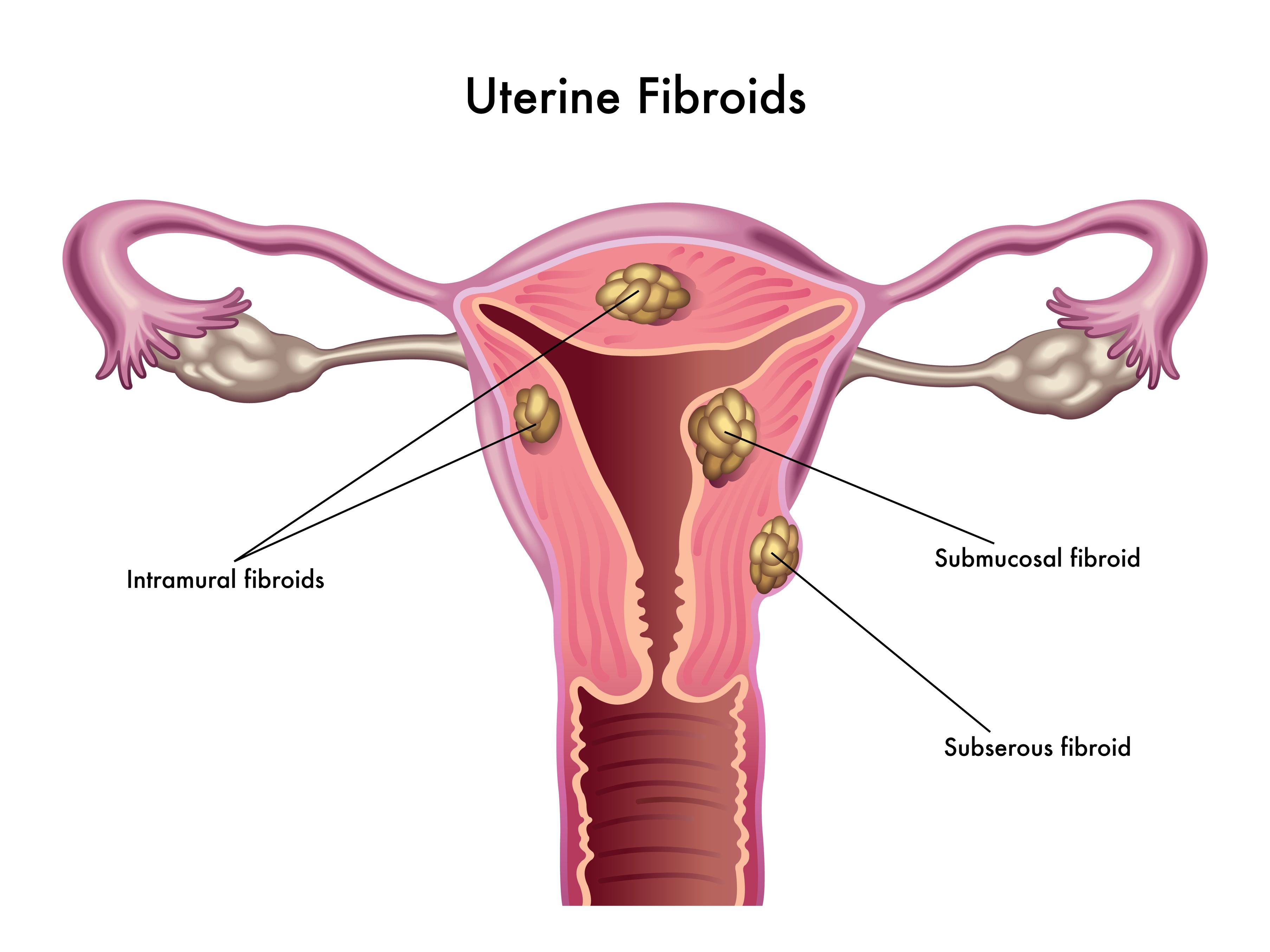
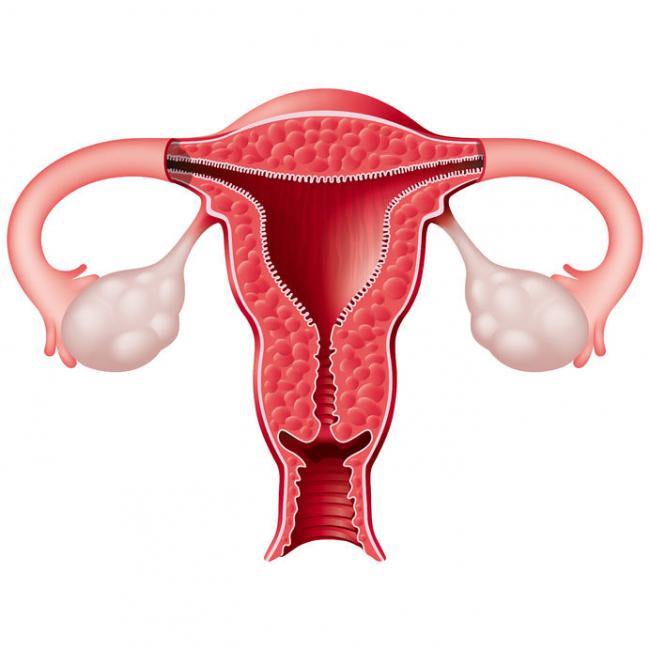
OVARIAN CYSTS
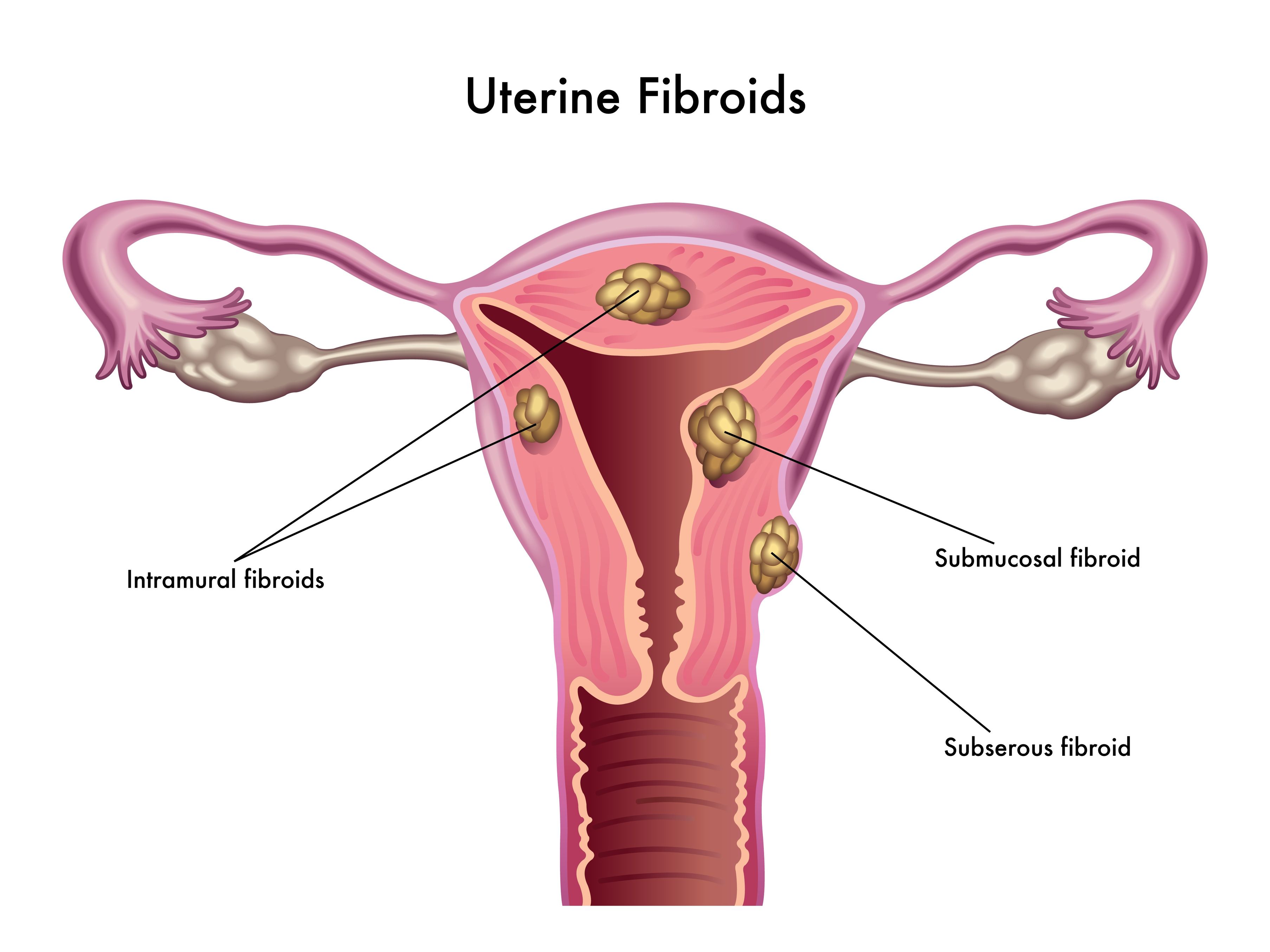
Ovarian cysts are much more common and discreet than breast cysts, but operate in much the same way. Every month there is a production of follicles in the first half of the ovarian cycle, that mature and release progesterone. If the egg is not fertilized, the process begins over again the next month. Sometimes, no egg is released from the ovary and therefore no rise in progesterone. The continued release of estrogen causes the cysts to continue developing in their sac and grow larger and larger (5).

Cysts can grow very large in response to high estrogen. Some women can notice them and feel them, others do not even know they exist. When an ovarian cysts ruptures, it can be incredibly painful and warrant a visit to the hospital. However, unless there is a workup from a medical doctor including and pelvic exam and ultrasound, cysts are generally undetected.
During the monthly cycle, cysts can create pain during ovulation and in the days leading up to the next period. Because everything in the lower abdomen swells with the flux of hormones, there is more pressure on an ovarian cyst, resulting in increased pain. Because cysts generally disappear after menopause, a full investigation is warranted for any cysts or lumps that develop in that time.
PMS MANAGEMENT
A PMS management plan must be individualized and specific to each person’s family history, hormone levels and lifestyle. The general trend for all the PMS factors listed here is a picture of high estrogen and insufficient or reduced progesterone. When we have too much estrogen and can’t eliminate, it starts to cause more problems. Without considering any vitamins or supplements, a significant change in hormone balance can be achieved simply with diet and exercise.
By limiting the amount of refined sugars and carbohydrates we can reduce inflammation in the body associated with increased menstrual cramping. Dairy products and meat are often treated with hormones and antibiotics, which we consume and elevate our own estrogen levels. Being cautious of the our meat choices can make a big difference in a short period of time.
Outside of diet, we know that estrogen is stored in fat tissue and that by exercising we mobilize fat stores. This is an important way to detoxify excess estrogen from the body as well as elevating mood and improving muscle mass. Lastly, the effect of stress on hormone levels cannot be ignored. Taking the time for ourselves, finding some peace and quiet and lowering stress levels can keep our hormones balanced without any medication.
REFERENCES
- A, Direkvand-Moghadam et al. “Epidemiology of Premenstrual Syndrome (PMS)-A Systematic Review and Meta-Analysis Study.” Journal of clinical and diagnostic research : JCDR vol. 8,2 (2014): 106-9. doi:10.7860/JCDR/2014/8024.4021
- WebMD (2020) Premenstrual Dysphoric Disorder. Different from PMS? Retrieved from: https://www.mayoclinic.org/diseases-conditions/premenstrual-syndrome/expert-answers/pmdd/faq-20058315
- Vanderhaeghe, L (2004) Premenstrual Syndrome. An A-Z Women’s Guide to Vibrant Health. pp 83-86
- Vanderhaeghe, L (2004) Anemia. An A-Z Women’s Guide to Vibrant Health. pp 11-14
Vanderhaeghe, L (2004) Ovarian Cysts, Polycystic Ovary Syndrome and Ovarian Cancer. An A-Z Women’s Guide to Vibrant Health. pp 70-74