Anxiety: Diet as Therapy
Anxiety: Diet as Therapy
by Jill Northrup
Considerations for the Approach to Anxiety Management
Anxiety is an extremely common mental-health diagnosis with systemic and long-term health consequences. As anxiety diagnoses become far more common among Canadians,[1] there is a need for therapies that are safer, more sustainable, and that target the root cause. Conventionally, psychotherapy and pharmacotherapy are the most utilized anxiety treatments.[2] Although highly effective for some, for others, these treatments are only partially effective or are unsustainable due to adverse effects or a lack of accessibility.[3]
In the naturopathic management of anxiety, various herbs and nutraceuticals are common treatments. Practitioners and patients alike often overlook the most fundamental modality as an adjunctive component of anxiety management: nutrition.
Anxiety can be directly influenced by different dietary components or eating patterns, and existing diagnoses can be exacerbated by nutritional habits. Nutrition is one of the most basic forms of medicine and, despite the impact of diet on overall health and the growing body of evidence to show its benefit for mental health, nutritional interventions are infrequently made in clinical practice.[4] This review will outline the role diet plays in the manifestation of anxiety and evidence-based nutritional strategies for managing anxiety.
Introduction to Nutritional Psychiatry
Many dietary constituents and patterns are associated with either protection against—or an increased risk of—anxiety. Anxiety is inversely correlated with a diet rich in fruits and vegetables and omega-3 fatty acids.[5] A reduction of anxiety is also associated with “healthy” dietary patterns, including the Mediterranean, vegetarian, and anti-inflammatory diets. Conversely, anxiety prevalence and severity are correlated with “unhealthy” eating paradigms, including a typical Western diet, which is associated with a high intake of saturated fat, refined carbohydrates, sugar, processed foods, and fast foods.[6]
Dietary patterns with an emphasis on whole, unprocessed foods, including a plethora of fruits and vegetables, whole grains, lean proteins, and healthy fats are protective, as they encompass a multitude of vitamins, minerals, and phytochemicals which modulate inflammation and support neurotransmitter synthesis.[7], [8] These nutrients include magnesium, zinc, B vitamins, vitamin C, vitamin E, and omega-3 fatty acids, among others.[9] These general guidelines are a good foundational approach to both mental health and overall wellness, but beyond the bare minimum of ensuring nutrient adequacy, other dietary factors influence mental health. Beyond these more basic principles, other, more specific—and perhaps insidious—components of the diet will also be examined.
Breakfast Consumption
 It’s a popular belief that breakfast is the most important meal of the day; however, does breakfast consumption impact mental health? A large systematic review and meta-analysis of 16,544 participants found that breakfast consumption had no correlation with anxiety incidence among adults but was significantly correlated with anxiety and psychological distress among adolescents.[10] Furthermore, the types of foods that were consumed for breakfast also played a role in mental wellbeing. Adolescents consuming a “high-quality” breakfast have significantly lower perceived stress and significantly greater health-related quality-of-life scores in comparison to those eating a “low-quality” breakfast.[11] High-quality breakfasts consisted of grains and dairy products and no commercially baked goods, and low-quality breakfasts consisted of commercially baked goods and no grains or dairy.[12]
It’s a popular belief that breakfast is the most important meal of the day; however, does breakfast consumption impact mental health? A large systematic review and meta-analysis of 16,544 participants found that breakfast consumption had no correlation with anxiety incidence among adults but was significantly correlated with anxiety and psychological distress among adolescents.[10] Furthermore, the types of foods that were consumed for breakfast also played a role in mental wellbeing. Adolescents consuming a “high-quality” breakfast have significantly lower perceived stress and significantly greater health-related quality-of-life scores in comparison to those eating a “low-quality” breakfast.[11] High-quality breakfasts consisted of grains and dairy products and no commercially baked goods, and low-quality breakfasts consisted of commercially baked goods and no grains or dairy.[12]
Overall, the evidence suggests consuming breakfast plays a larger role in the mental health of adolescents, and a lesser one for adults. However, due to the other health benefits of a morning meal, including a reduced risk of obesity [13] and fatigue and increased concentration,[14] breakfast may be an important meal to incorporate for all age groups.
Caffeine
 Caffeine also has the potential to cause or exacerbate anxiety. As a central nervous–system stimulant, caffeine readily crosses the blood-brain barrier and increases the production of catecholamines, hormones involved in the fight-or-flight stress response.[15] A double-blind study examining the impact of varying doses of caffeine on stress and anxiety found that following caffeine administration, anxiety, depression, and hostility scores were significantly increased in a dose-dependent manner.[16]
Caffeine also has the potential to cause or exacerbate anxiety. As a central nervous–system stimulant, caffeine readily crosses the blood-brain barrier and increases the production of catecholamines, hormones involved in the fight-or-flight stress response.[15] A double-blind study examining the impact of varying doses of caffeine on stress and anxiety found that following caffeine administration, anxiety, depression, and hostility scores were significantly increased in a dose-dependent manner.[16]
Coffee is one of the most caffeine-dense sources, at 135 mg of caffeine per cup.[17] Black and green teas also contain caffeine (30–50 mg per cup), as do many soft drinks (40–50 mg per 355 ml can), and smaller quantities are found in chocolate and decaffeinated coffee.[18] The effects of caffeine consumed in the form of coffee can be more difficult to distinguish and interpret due to the presence of various other compounds;[19] however, coffee consumption and anxiety are correlated, though individual tolerance also impacts the effects of caffeine. Those consuming little to no caffeine in the form of coffee, and those prone to anxiety, are perhaps more susceptible to the anxiety-producing effects of caffeine than those who consume coffee regularly. Individuals with anxiety often improve following caffeine elimination; however, initial caffeine withdrawal may exacerbate anxiety symptoms.[20]
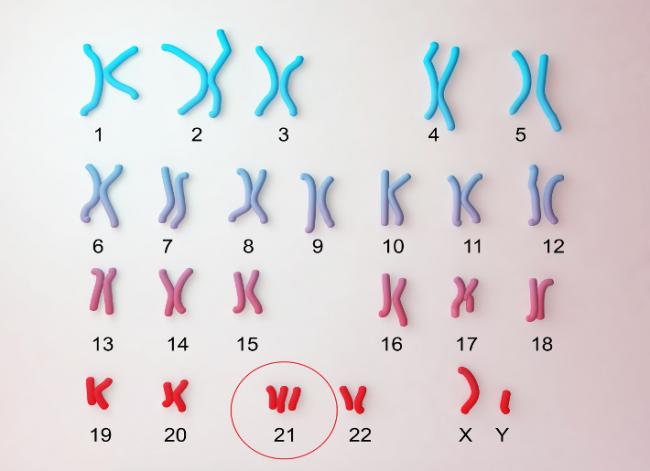
Many factors influence the metabolism and effects of caffeine. Metabolism is controlled by the CYP1A2 gene, and variations in this gene account for varying rates of caffeine metabolism.[21] Those with CYP1A2 variations contributing to a slower metabolism are more likely to experience more intense and prolonged effects of caffeine.[22] Although genetics are a nonmodifiable factor determining response to caffeine, its effects can be somewhat mitigated by combining food with caffeine ingestion. The presence of food in the gastrointestinal tract, especially fibrous foods, can significantly reduce the speed of absorption, thereby mitigating the anxiety-related effects of caffeine.[23] Lastly, it is also important to note that caffeine can interact with some pharmaceuticals to produce increased levels of anxiety. Most notably, benzodiazepines, a medication class prescribed for anxiety, can increase anxiety and panic when combined with caffeine.[24] Overall, depending on individual sensitivity, the reduction or complete elimination of caffeine may be a useful strategy in reducing symptoms of anxiety.[25]
Macronutrients: Carbohydrates, Proteins, and Fats
Carbohydrates
As previously noted, higher intakes of simple and refined carbohydrates, high-glycemic-index foods, and sugar are associated with increased anxiety.[26], [27], [28] This relationship is bidirectional. First, following consumption of a high-glycemic-index food (e.g., white breads, pasta, potatoes, and sugary foods), rapid hyperglycemia results, stimulating mass insulin release, producing subsequent hypoglycemia.[29] Anxiety and nervousness are among the symptoms of hypoglycemia, in addition to fatigue and hunger. These symptoms act as a physiological safety mechanism to stimulate feeding in an effort to stabilize blood glucose. With repeated bouts of hyperglycemia, insulin sensitivity declines, producing a lower threshold for the generation of these symptoms.[30]
Secondly, those suffering from anxiety are also predisposed to carbohydrate cravings, as carbohydrates relieve anxiety through increasing serotonin production.[31] Unfortunately, the anxiolytic effect of this self-soothing behaviour is short-lived and only further perpetuates the cycle of hyperglycemia, subsequent hypoglycemia, and anxiety.
Although it can be difficult to distinguish whether feeding behaviour or anxiety is the initial catalyst of this cycle, reduction of high-glycemic-index foods and carbohydrates in general is beneficial among those experiencing anxiety.[32], [33] Furthermore, combining protein and fats along with carbohydrates can also help mitigate hypoglycemia-induced anxiety, as the presence of protein and fat help to slow the absorption of glucose from carbohydrates, which dampens insulin release.[34]
Protein
Protein, independent of its impact on blood glucose, is also a key macronutrient for managing anxiety. The essential amino acid tryptophan is required for serotonin synthesis.[35] Tryptophan-depleted individuals experience increased anxiety, which can be relieved with tryptophan supplementation. A ketogenic diet, which is characterized by a high protein intake, is also associated with reduced anxiety,[36] although additional studies are required before this diet can become a staple of anxiety treatment.[37]
Again, adolescents seem particularly vulnerable to this dietary component. Adolescents consuming sufficient and high-quality protein are significantly less likely to experience anxiety, compared to those consuming insufficient or poor-quality proteins.[38] Protein consumption also had a significant dose-dependent relationship with incidence of anxiety: Individuals with borderline anxiety consumed less protein than those without anxiety, and those with clinically significant anxiety symptoms consumed less protein than those with borderline anxiety.[39] A higher-quality–protein diet includes more plant proteins and fewer animal proteins,[40] and is characterized by completeness in amino-acid composition.[41]
In the context of anxiety, protein adequacy should be achieved as well as proper timing of protein in relationship to carbohydrates, utilizing high-quality–protein sources
Fat
 The most relevant forms of fat, when examining mental health, are omega‑3s. Omega‑3 fatty acids are associated with a reduction in anxiety, whereas trans fats and diets high in fat and cholesterol in general are associated with greater anxiety.[42]
The most relevant forms of fat, when examining mental health, are omega‑3s. Omega‑3 fatty acids are associated with a reduction in anxiety, whereas trans fats and diets high in fat and cholesterol in general are associated with greater anxiety.[42]
Omega‑3s are anti-inflammatory and help to maintain cell structure and integrity as a crucial component of the cell membrane.[43] The omega‑3 fatty acids include alpha-lipoic acid (ALA), docosahexaenoic acid (DHA), and eicosapentaenoic acid (EPA). DHA is the primary omega‑3 within the brain and is the most relevant fatty acid for proper brain development and cognitive function.[44] DHA can be produced from ALA and EPA in the liver; however, conversion rates are limited and only yield a fraction of DHA.[45] This emphasizes the importance of obtaining DHA from the diet. DHA consumption has been found to be inversely correlated with anxiety, with individuals who consume over 270 mg/d of DHA being 50% less likely to have an anxiety disorder than those consuming less.[46]
Examining omega‑3 consumption in general, individuals consuming between 0.87 and 1.17 g/d of omega‑3 fatty acids had a relative risk reduction of over 30% of developing a mental-health diagnosis, including anxiety, after a two-year period.[47] Individuals consuming this average fatty acid intake also consumed between 83 and 112 g/d of fish.[48] Fish are one of the richest sources of omega‑3 fatty acids, with salmon containing approximately 1.24 g of DHA and 0.59 g of EPA per 3 ounces, a serving size approximately the size of a palm.[49] Other sources of EPA and DHA include sardines, mackerel, and trout. ALA‑rich foods include flaxseed oil, soybean oil, chia seeds, walnuts, and canola oil. Individuals looking to manage anxiety through diet should consider incorporating sources of omega‑3 fatty acids on a regular basis, especially DHA.
Probiotic and Prebiotic Foods
 The composition of the gut microbiome also plays a role in stress and anxiety. Through direct communication with the brain via the vagal nerve, the gastrointestinal microbiota can directly influence mental wellbeing and vice versa: This is known as the gut–brain axis.[50], [51] Imbalances in gut flora, referred to as intestinal dysbiosis, have been correlated with anxiety,[52] as has antibiotic usage.[53] Conditions associated with dysbiosis, including small intestinal bacterial overgrowth (SIBO) and irritable bowel syndrome (IBS), are also commonly comorbid with anxiety.[54] In fact, stress alone can alter gut flora.[55] Harmful flora, present in greater quantities in dysbiosis, are proposed to interfere with tryptophan metabolism and reduce serotonin synthesis, thereby inducing anxiety.[56] As the gut produces over 95% of the body’s serotonin, this is significant.[57]
The composition of the gut microbiome also plays a role in stress and anxiety. Through direct communication with the brain via the vagal nerve, the gastrointestinal microbiota can directly influence mental wellbeing and vice versa: This is known as the gut–brain axis.[50], [51] Imbalances in gut flora, referred to as intestinal dysbiosis, have been correlated with anxiety,[52] as has antibiotic usage.[53] Conditions associated with dysbiosis, including small intestinal bacterial overgrowth (SIBO) and irritable bowel syndrome (IBS), are also commonly comorbid with anxiety.[54] In fact, stress alone can alter gut flora.[55] Harmful flora, present in greater quantities in dysbiosis, are proposed to interfere with tryptophan metabolism and reduce serotonin synthesis, thereby inducing anxiety.[56] As the gut produces over 95% of the body’s serotonin, this is significant.[57]
However, diet can improve microbial diversity in the gut. Diets rich in fibre and fermented foods as sources of prebiotics and probiotics, respectively, are associated with reduced anxiety severity.[58] Psychobiotics, strains and species that are associated with protective mental-health effects, are proposed to have anti-inflammatory activity, modulate the HPA axis responsible for the stress response, regulate and support neurotransmitter synthesis, and increase the synthesis of calming B vitamins to promote anxiolytic effects.[59] In particular, sources of Lactobacilli and Bifidobacteria are proposed to have the greatest mental health benefits.[60], [61]
Supplementation with probiotics in the treatment of anxiety shows they may be of some benefit; however, most meta-analyses conclude that more primary research is required before probiotics can become a mainstay recommendation for anxiety.[62], [63], [64], [65] Research also suggests that modifying microbiome through diet to treat anxiety is perhaps more effective than probiotic supplementation.[66] Incorporation of probiotic and prebiotic foods into the diet can promote microbial diversity.[67] Probiotic foods include fermented foods such as kimchi, sauerkraut, kombucha, and kefir, which contain various microbial species. Prebiotic foods are soluble dietary fibre found in fruits and vegetables, including asparagus, leeks, and bananas, as well as oats and wheat.[68] In the gut, fibre is fermented into short-chain fatty acids, including butyrate, which regulate the integrity of the intestinal epithelium and nourish intestinal epithelial cells and good microbes.[69]
Dietary patterns that promote overall microbial diversity include the Mediterranean and ketogenic diets, in contrast to a Western diet, which reduces microbial diversity.[70] Overall, food sources of prebiotics and probiotics may be an important consideration for those with anxiety, especially those with intestinal dysbiosis.
Gluten
 For some individuals who are sensitive, gluten can also cause or exacerbate anxiety. Celiac disease is an intolerance to gluten, mediated by an IgE immune reaction to gluten proteins found in wheat.[71] The mechanism by which gluten consumption among those intolerants is believed to contribute to anxiety includes both micronutrient deficiencies due to malabsorption in the gut and hyperhomocysteinemia.[72] Gluten consumption among celiacs is also believed to interfere with serotonin synthesis, reflected by low circulating tryptophan; removal of gluten from the diet is associated with normalization of ʟ‑tryptophan levels.[73] Overall, upon initiating a gluten-free diet, celiac patients experience a significant reduction of anxiety.[74]
For some individuals who are sensitive, gluten can also cause or exacerbate anxiety. Celiac disease is an intolerance to gluten, mediated by an IgE immune reaction to gluten proteins found in wheat.[71] The mechanism by which gluten consumption among those intolerants is believed to contribute to anxiety includes both micronutrient deficiencies due to malabsorption in the gut and hyperhomocysteinemia.[72] Gluten consumption among celiacs is also believed to interfere with serotonin synthesis, reflected by low circulating tryptophan; removal of gluten from the diet is associated with normalization of ʟ‑tryptophan levels.[73] Overall, upon initiating a gluten-free diet, celiac patients experience a significant reduction of anxiety.[74]
For other individuals with a gluten sensitivity as opposed to intolerance, gluten can be a more insidious cause of their anxiety symptoms. Gluten sensitivity is six times more prevalent than celiac disease, but more difficult to diagnose than celiac due to vague systemic symptoms as well as a lack of standardized testing.[75] Gluten sensitivity is both an underdiagnosed and undertreated issue.[76] Similar to celiac patients, gluten ingestion has been shown to aggravate mood disorders including anxiety, even among patients with a nonceliac gluten sensitivity.[77]
As part of an in-depth dietary management approach to anxiety, gluten should be considered as a potential culprit, especially for those who experience intestinal and extraintestinal symptoms in addition to anxiety.
Conclusion
In general, the impact of diet on mental wellbeing is undeniable. As an increasingly prevalent diagnosis, practitioners and patients are looking for new ways to manage anxiety. As the body of research in the field of nutritional psychiatry grows, recommendations can move away from the general dietary advice of “consume more fruits and vegetables and reduce processed foods,” and can focus on aspects of diet that are less understood and widely accepted by the general public. Ultimately, the field of nutritional psychiatry emphasizes the importance of naturopathic medicine and the holistic approach, while also empowering the public to take their health into their own hands—and onto their own plates.
References
References
[1] Statistics Canada. Survey on COVID-19 and Mental Health, February to May 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/210927/dq210927a-eng.htm · Released 2021-09-27.
[2] Aucoin, M., L. LaChance, U. Naidoo, D. Remy, T. Shekdar, N. Sayar, V. Cardozo, T. Rawana, I. Chan, and K. Cooley. “Diet and anxiety: A scoping review.” Nutrients, Vol. 13, No. 12 (2021): 4418.
[3] Aucoin et al, op. cit.
[4] Aucoin et al, op. cit.
[5] Aucoin et al, op. cit.
[6] Aucoin et al, op. cit.
[7] Aucoin et al, op. cit.
[8] Kris‑Etherton, P.M., K.S. Petersen, J.R. Hibbeln, D. Hurley, V. Kolick, S. Peoples, N. Rodriguez, and G. Woodward‑Lopez. “Nutrition and behavioral health disorders: Depression and anxiety.” Nutrition Reviews, Vol. 79, No. 3 (2021): 247–260.
[9] Kris-Etherton et al, op. cit.
[10] Zahedi, H., S. Djalalinia, O. Sadeghi, F. Zare Garizi, H. Asayesh, M. Payab, M. Zarei, and M. Qorbani. “Breakfast consumption and mental health: A systematic review and meta-analysis of observational studies.” Nutritional Neuroscience, Vol. 25, No. 6 (2022): 1250–1264.
[11] Ferrer‑Cascales, R., M. Sánchez‑SanSegundo, N. Ruiz‑Robledillo, N. Albaladejo‑Blázquez, A. Laguna‑Pérez, A. Zaragoza‑Martí. “Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in Spanish adolescents.” International Journal of Environmental Research and Public Health, Vol. 15, No. 8 (2018): 1781.
[12] Ferrer-Cascales et al, op. cit.
[13] Ma, X., Q. Chen, Y. Pu, M. Guo, Z. Jiang, W. Huang, Y. Long, and Y. Xu. “Skipping breakfast is associated with overweight and obesity: A systematic review and meta-analysis.” Obesity Research & Clinical Practice, Vol. 14, No. 1 (2020): 1–8.
[14] Ackuaku‑Dogbe, E.M., and B. Abaidoo. “Breakfast eating habits among medical students.” Ghana Medical Journal, Vol. 48, No. 2 (2014): 66–70.
[15] Papadelis, C., C. Kourtidou‑Papadeli, E. Vlachogiannis, P. Skepastianos, P. Bamidis, N. Maglaveras, and K. Pappas. “Effects of mental workload and caffeine on catecholamines and blood pressure compared to performance variations.” Brain and Cognition, Vol. 51, No. 1 (2003): 143–154.
[16] Veleber, D.M., and D.I. Templer. “Effects of caffeine on anxiety and depression.” Journal of Abnormal Psychology, Vol. 93, No. 1 (1984): 120–122.
[17] Health Canada. Caffeine in foods. https://www.canada.ca/en/health-canada/services/food-nutrition/food-safety/food-additives/caffeine-foods.html · Updated 2022‑07‑20.
[18] Health Canada, op. cit.
[19] Nehlig, A., J.L. Daval, and G. Debry. “Caffeine and the central nervous system: Mechanisms of action, biochemical, metabolic and psychostimulant effects.” Brain Research Reviews, Vol. 17, No. 2 (1992): 139–170.
[20] Nehlig, Daval, and Debry, op. cit.
[21] Temple, J.L., C. Bernard, S.E. Lipshultz, J.D. Czachor, J.A. Westphal, and M.A. Mestre. “The safety of ingested caffeine: A comprehensive review.” Frontiers in Psychiatry, Vol. 8 (2017): 80.
[22] Temple et al, op. cit.
[23] Institute of Medicine (US). Caffeine for the sustainment of mental task performance: formulations for military operations. Washington, DC: National Academy Press, 2001.
[24] Nehlig, Daval, and Debry, op. cit.
[25] Health Canada, op. cit.
[26] Aucoin et al, op. cit.
[27] Kose, J., L.K. Fezeu, M. Touvier, S. Péneau, S. Hercberg, P. Galan, and V.A. Andreeva. “Dietary macronutrient intake according to sex and trait anxiety level among non-diabetic adults: A cross-sectional study.” Nutrition Journal, Vol. 20, No. 1 (2021): 78.
[28] Daneshzad, E., S.A. Keshavarz, M. Qorbani, B. Larijani, and L. Azadbakht. “Association between a low‐carbohydrate diet and sleep status, depression, anxiety, and stress score.” Journal of the Science of Food and Agriculture, Vol. 100, No. 7 (2020): 2946–2952.
[29] Gangwisch, J.E., L. Hale, L. Garcia, D. Malaspina, M.G. Opler, M.E. Payne, R.C. Rossom, and D. Lane. “High glycemic index diet as a risk factor for depression: Analyses from the Women’s Health Initiative.” The American Journal of Clinical Nutrition, Vol. 102, No. 2 (2015): 454–463.
[30] Gangwisch et al, op. cit.
[31] Ventura, T., J. Santander, R. Torres, and A.M. Contreras. “Neurobiologic basis of craving for carbohydrates.” Nutrition, Vol. 30, No. 3 (2014): 252–256.
[32] Aucoin et al, op. cit.
[33] Aucoin, M., and S. Bhardwaj. “Generalized anxiety disorder and hypoglycemia symptoms improved with diet modification.” Case Reports in Psychiatry, Vol. 2016 (2016): 7165425.
[34] Aucoin and Bhardwaj, op. cit.
[35] Aucoin et al, op. cit.
[36] Aucoin et al, op. cit.
[37] Włodarczyk, A., W.J. Cubała, and A. Wielewicka. “Ketogenic diet: A dietary modification as an anxiolytic approach?” Nutrients, Vol. 12, No. 12 (2020): 3822.
[38] Khanna, P., and B.T. Aeri. “Association of quantity and quality of protein intake with depression and anxiety symptoms among adolescent boys and girls (13–15 years) studying in public schools of Delhi.” Journal of Nutritional Science and Vitaminology, Vol. 66 Supplement (2020): S141–S148.
[39] Khanna and Aeri, op. cit.
[40] Sheikhi, A., F. Siassi, A. Djazayery, B. Guilani, and L. Azadbakht. “Plant and animal protein intake and its association with depression, anxiety, and stress among Iranian women.” BMC Public Health, Vol. 23, No. 1 (2023): 161.
[41] Khanna and Aeri, op. cit.
[42] Aucoin et al, op. cit.
[43] National Institutes of Health. Office of Dietary Supplements. Omega‑3 Fatty Acids. Fact Sheet for Health Professionals. https://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/ · Updated 2023‑02‑15.
[44] Horrocks, L.A., and Y.K. Yeo. “Health benefits of docosahexaenoic acid (DHA).” Pharmacological Research, Vol. 40, No. 3 (1999): 211–225.
[45] National Institutes of Health, op. cit.
[46] Jacka, F.N., J.A. Pasco, L.J. Williams, B.J. Meyer, R. Digger, and M. Berk. “Dietary intake of fish and PUFA, and clinical depressive and anxiety disorders in women.” British Journal of Nutrition, Vol. 109, No. 11 (2013): 2059–2066.
[47] Sanchez-Villegas, A., P. Henríquez, A. Figueiras, F. Ortuño, F. Lahortiga, and M.A. Martínez‑González. “Long chain omega‑3 fatty acids intake, fish consumption and mental disorders in the SUN cohort study.” European Journal of Nutrition, Vol. 46, No. 6 (2007): 337–346.
[48] Sanchez-Villegas et al, op. cit.
[49] National Institutes of Health, op. cit.
[50] Cryan, J.F., K.J. O’Riordan, C.S. Cowan, K.V. Sandhu, T.F. Bastiaanssen, M. Boehme, M.G. Codagnone, et al. “The microbiota-gut-brain axis.” Physiological Reviews, Vol. 99, No. 4 (2019): 1877–2013.
[51] Vitellio, P., A. Chira, M. De Angelis, D.L. Dumitrascu, and P. Portincasa. “Probiotics in psychosocial stress and anxiety. A systematic review.” Journal of Gastrointestinal & Liver Diseases, Vol. 29, No. 1 (2020): 77–83.
[52] Shafiq, J., B. Khan, F. Saleem, G. Abbas, and A. Ahmed. “Gut microbiome interferes with host tryptophan metabolism pathway and regulate basal anxiety–like behavior.” International Journal of Infectious Diseases, Vol. 101, Suppl. 1 (2020): 5.
[53] Aucoin et al, op. cit.
[54] Addolorato, G., A. Mirijello, C. D’Angelo, L. Leggio, A. Ferrulli, L. Abenavoli, L. Vonghia, et al. “State and trait anxiety and depression in patients affected by gastrointestinal diseases: Psychometric evaluation of 1641 patients referred to an internal medicine outpatient setting.” International Journal of Clinical Practice, Vol. 62, No. 7 (2008): 1063–1069.
[55] Cryan et al, op. cit.
[56] Shafiq et al, op. cit.
[57] Terry, N., and K.G. Margolis. “Serotonergic mechanisms regulating the GI tract: Experimental evidence and therapeutic relevance.” Gastrointestinal Pharmacology, Vol. 239 (2017): 319–342.
[58] Aucoin et al, op. cit.
[59] Aslam, H., J. Green, F.N. Jacka, F. Collier, M. Berk, J. Pasco, and S.L. Dawson. “Fermented foods, the gut and mental health: A mechanistic overview with implications for depression and anxiety.” Nutritional Neuroscience, Vol. 23, No. 9 (2020): 659–671.
[60] Vitellio et al, op. cit.
[61] Aucoin et al, op. cit.
[62] Vitellio et al, op. cit.
[63] Chao, L., C. Liu, S. Sutthawongwadee, Y. Li, W. Lv, W. Chen, L. Yu, et al. “Effects of probiotics on depressive or anxiety variables in healthy participants under stress conditions or with a depressive or anxiety diagnosis: A meta-analysis of randomized controlled trials.” Frontiers in Neurology, Vol. 11 (2020): 421.
[64] Liu, R.T., R.F. Walsh, and A.E. Sheehan. “Prebiotics and probiotics for depression and anxiety: A systematic review and meta-analysis of controlled clinical trials.” Neuroscience & Biobehavioral Reviews, Vol. 102 (2019): 13–23.
[65] Huang, R., H. Ning, L. Yang, C. Jia, F. Yang, G. Xu, and H. Tan. “Efficacy of probiotics on anxiety: A meta-analysis of randomized controlled trials.” Neuropsychiatry, Vol. 7, No. 6 (2017): 862–871.
[66] Yang, B., J. Wei, P. Ju, and J. Chen. “Effects of regulating intestinal microbiota on anxiety symptoms: A systematic review.” General Psychiatry, Vol. 32, No. 2 (2019): e100056.
[67] Cryan et al, op. cit.
[68] Cryan et al, op. cit.
[69] Taylor, A.M., and H.D. Holscher. “A review of dietary and microbial connections to depression, anxiety, and stress.” Nutritional Neuroscience, Vol. 23, No. 3 (2020): 237–250.
[70] Cryan et al, op. cit.
[71] Jackson, J.R., W.W. Eaton, N.G. Cascella, A. Fasano, and D.L. Kelly. “Neurologic and psychiatric manifestations of celiac disease and gluten sensitivity.” Psychiatric Quarterly, Vol. 83, No. 1 (2012): 91–102.
[72] Trovato, C.M., U. Raucci, F. Valitutti, M. Montuori, M.P. Villa, S. Cucchiara, and P. Parisi. “Neuropsychiatric manifestations in celiac disease.” Epilepsy & Behavior, Vol. 99 (2019): 106393.
[73] Jackson et al, op. cit.
[74] Jackson et al, op. cit.
[75] Jackson et al, op. cit.
[76] Jackson et al, op. cit.
[77] Busby, E., J. Bold, L. Fellows, and K. Rostami. “Mood disorders and gluten: It’s not all in your mind! A systematic review with meta-analysis.” Nutrients, Vol. 10, No. 11 (2018): 1708.