Related Articles
- 15 Jun 21
Medium-chain triglycerides, or MCTs, have been popularized in the context of Bulletproof™ coffee or the ketogenic diet. MCTs and the keto diet have been investigated in the management of obesity, insulin resistance, , epilepsy, neurodegenerative conditions, and others.
- 27 Jan 21Emerging health implications of gluten sensitivity reach far beyond the borders of the gastrointestinal tract. The gluten-sensitive spectrum includes different forms of manifestations: allergic (wheat allergy), autoimmune celiac disease (CD), dermatitis herpetiformis, gluten ataxia, and immune-mediated (nonceliac gluten sensitivity).
- 12 Feb 20
Endometriosis is one of the most common chronic gynecological conditions in women of reproductive age. Not only is it associated with severe, debilitating pain, but it can also have significant implications for a woman’s fertility.[1]
- 29 Jan 21Adrenal fatigue affects individuals who suffer from a long stretch of physical, mental, environmental, or emotional stress. A “long stretch” can be defined as greater than three months. Adrenal fatigue can affect anyone, but individuals who are more likely to suffer from adrenal fatigue include single parents, individuals who are drug-dependent, those who have faced a life crisis or trauma, or those who have a stressful job circumstance.
- 29 Jan 24
The article explores how dietary choices impact anxiety, from breakfast habits to macronutrients like carbohydrates and proteins. It also highlights the role of gut health and gluten sensitivity in mental wellbeing.
- 27 Sep 21
Throughout the ages, humans have searched for the Fountain of Youth. Today, the search for eternal youth continues; however, we are no longer looking for a hidden fountain but instead, for lifestyle, dietary, and technological hacks we can use in attempts to delay the aging process.
- 28 Jan 21Advanced glycation end-products (AGEs) are compounds that are generated under hyperglycemic conditions. They could be formed endogenously, or they could be consumed from our diet. Increased presence of AGEs in the human body is associated with diverse age-related and chronic conditions...
- 09 Jan 20
Fasting has been around for generations as part of cultural spiritual practices. Today, it is used for proper weight maintenance, healing from disease, and prevention. Humans are metabolically flexible: We are able to change the source of energy that we use to power our cells depending on the available resources. Ultimately, it is the production of ketones that generates the healing ability of a fast, disease prevention, and increased longevity.
- 13 Apr 20
Bone is our main structural support system. It allows us to protect our vital organs, facilitates movement, and creates a scaffold for blood vessels and nerves. In additional to the structural functions, bone has important metabolic and endocrine functions as well.
- 12 Feb 20
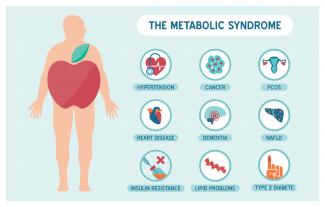
Metabolic syndrome is a cluster of risk factors that increase one’s chances of developing serious illnesses in the future. Metabolic syndrome doubles the chance of developing cardiovascular disease while increasing the risk of diabetes, fatty liver, and several types of cancers.[1][2]
- 09 Jan 20
Premenstrual symptoms affect up to 80% of women. For many, these symptoms are bothersome but do not necessarily impact their daily functioning. Premenstrual syndrome (PMS), however, affects up to 20% of women. This diagnosis is defined by a woman’s experience of at least one physical and one psychiatric symptom each month in the second half of her cycle (7–14 days before her period), that alleviate with or shortly after the onset of menses.
- 10 Jun 20
By now, most of us have heard the word microbiome—the collection of trillions of functional bacteria of all different species found in many places throughout our bodies, such as our skin, gut, mouth, vagina, and lungs.
- 09 Jan 20
What is ketosis and the keto diet? Is it good for you, or is it just another lifestyle trend that we’ll forget about in a few years? In this article, we’ll try to answer this question and review the available evidence to see what we can learn.
- 12 Feb 20
Mild traumatic brain injuries (mTBIs) and postconcussion syndrome are becoming more of a public health concern. Although termed “mild,” the effects can certainly be debilitating and severe in some cases. The symptoms of postconcussion syndrome include headaches, memory and concentration difficulties, irritability, fatigue, nausea, visual disturbances, light and noise sensitivity, judgement problems, depression, and anxiety.
- 09 Mar 20
The viruses that cause colds and the flu can be spread easily by coughing and sneezing. While there is no way to guarantee you won’t get sick this winter, there are things you can do to reduce the severity of your sickness.
- 05 May 20
Acne (or acne vulgaris) is one of the most common skin conditions, affecting 64% of people in their 20s and 43% of people in their 30s. It affects the pilosebaceous units of the skin, which is essentially the oil gland and hair follicle. It usually affects the largest, hormone-responsive sebaceous glands such as those on the face, chest, neck and back.
- 08 Jul 20
Anxiety is a very common mental-health disorder and can have implications on all aspects of one’s life. This may come from a variety of factors such as finances, relationships, health, and more. Anxiety lends itself well to natural treatments such as herbal medicine, supplements, and lifestyle modification
- 09 Jan 20
There are various supports for headache management such as supplements, acupuncture/body work, and herbal medicine.
Headaches can be divided into different categories, determining treatment type. - 13 Apr 20
Itchy skin, dryness, redness, and cracking—uncomfortable signs of an eczema flare-up that can range from mild to having a significant impact on quality of life. Corticosteroid creams can do a fine job of targeting symptoms and inflammation associated with eczema, although below are some suggestions to get to the root cause and prevent future flare-ups.
- 07 Aug 20
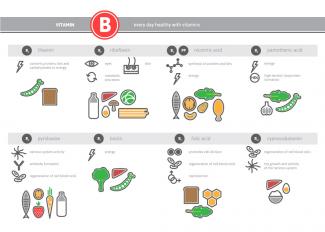
We know that vitamins play an important role in our energy and daily metabolic functions. We know that eating a balanced diet full of fruits and vegetables can help lower the risk of chronic disease and support brain functions. B vitamins are crucial to brain health and can reduce the intensity of mental illness, including symptoms relating to anxiety, depression, and chronic fatigue.
Newsletter
Most Popular
- 09 Jul 15
- 13 Feb 16
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13