Naturopathic Approaches to Heart Health
 Long before February was declared “Heart Month” in Canada, “American Heart Month” in the United States, and “National Heart Month” in the United Kingdom, children and adults celebrated February 14 as a day of love and affection. In addition to having the heart as a common symbol for these events, science has validated the connection of mood and a healthy heart. February is a good month to remember the wide range of naturopathic interventions that promote all things related to the heart.
Long before February was declared “Heart Month” in Canada, “American Heart Month” in the United States, and “National Heart Month” in the United Kingdom, children and adults celebrated February 14 as a day of love and affection. In addition to having the heart as a common symbol for these events, science has validated the connection of mood and a healthy heart. February is a good month to remember the wide range of naturopathic interventions that promote all things related to the heart.
The Heart and the Cardiovascular System
The cardiovascular system is a complex system, with the heart at its center, delivering oxygen-rich blood to the organs via a network of blood vessels. This system could be better understood using “the water-tower analogy of the cardiovascular system.”1 In this analogy, the heart is the city’s water tower that receives clean water before redistributing it to the appropriate local homes via distribution pipes. The water tower has sensors that allow it to monitor how much water is to be distributed to which house. The functioning of the water tower is dependent on the proper functioning of the clean-water supply as well as the integrity of the pipes and homes. As in this water-tower analogy, the proper functioning of the cardiovascular system is dependent on the organs that supply it oxygen-rich blood, the heart, the blood vessels, and the organs that need the blood.
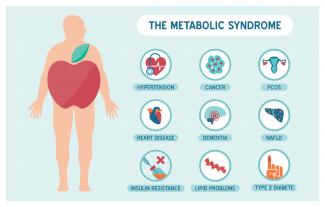
Cardiovascular health is evaluated with a variety of tools that give us information on the integrity of the heart muscles, heart valves, blood vessels, blood flow through the vessels, inflammation, and more. An impaired cardiovascular system could lead to a range of conditions including high blood pressure, atherosclerosis, arrhythmia, heart failure, stroke, and heart attack.
As in the water-tower analogy, heart health must be considered holistically. While genetic influences on cardiovascular health cannot be modified, lifestyle and natural medicine have been shown to modify cardiovascular outcomes. Below are some of the best-researched interventions for a healthy cardiovascular system.
The Power of Lifestyle Modifications
It is well established that exercise,2 diets rich in fruits and vegetables,3 vegetarian diets,4 the Mediterranean diet,5 and the Dietary Approaches to Stop Hypertension (DASH) diet 6 improve cardiovascular risk factors. Tobacco use is related to an increased risk of cardiovascular disease, while smoking cessation at an early age (40 years) has an impressive 90% reduction in the excess risk of death.7
The potential contribution of mood, sleep, sauna and bathing, and environment on cardiovascular health are often overlooked. Recent clinical research illustrates the significant impact of these lifestyle modifications on cardiovascular health and wellbeing.
 Mood
Mood
Positive psychological outlook including happiness, optimism, and gratitude are independently linked to improved cardiovascular health.8, 9 In a prospective study of 70,021 older women followed over eight years, women in the highest quartile of optimism had a 38% reduced risk (95% CI: 0.50 to 0.76) of heart-disease mortality and a 39% reduced risk (95% CI: 0.43 to 0.85) of stroke mortality.10
Interventions such as brief gratitude interventions (usually in the form of letters, journaling, and lists), the Best Possible Self exercise, and mindfulness meditation (such as the relaxation response), that improve subjective wellbeing and optimism, have favourable effects on the cardiovascular system.11, 12, 13
Sleep
The 24‑hour circadian clock regulates various cardiovascular functions including endothelial function, thrombus formation, blood pressure, and heart rate. Disruption of this rhythm has been associated with an increased incidence of cardiovascular disease including atherosclerosis, heart failure, myocardial infarction, and arrythmias.14, 15 Short-term circadian misalignment (12 h inverted cycle for three days) has been shown to increase 24 h systolic blood pressure and diastolic blood pressure by 3 mmHg and 1.5 mmHg, respectively, and increased inflammatory markers (serum interleukin‑6, C‑reactive protein, resistin, and tumour necrosis factor (TNF)‑α) levels by 3–29%.16
Consistent timing of sleep initiation and waking, sleeping in the dark, and other healthy sleep-hygiene practices could help to prevent circadian disruption and their effect on the cardiovascular system.
Sauna and Bathing
Sauna bathing and hot-water (> 41 °C) bathing are correlated with improved cardiovascular health.17 Hot-water bathing with a mean duration of 12.4 ± 9.9 min with a frequency of five times or more per week showed favourable effects on atherosclerotic and central haemodynamic parameters.18 In a prospective cohort study that followed 2,315 middle-aged men with a means follow‑up of 20.7 years, increased frequency of sauna bathing was associated with a reduced risk of sudden cardiac death, fatal coronary heart disease, fatal cardiovascular disease, and all-cause mortality.19 Another study, involving 102 participants, demonstrated that sauna bathing for 30 minutes had beneficial effects on arterial stiffness and blood pressure.20
Forest Bathing
Forest bathing encourages the “five-sense experience” (vision, smell, hearing, touch, and taste) when the body is exposed to a forest environment. A systematic review of forest bathing demonstrated that forest-bathing activities may have the following merits: remarkably improving cardiovascular function, hemodynamic indexes, and inflammatory indexes; significantly enhancing emotional state, attitude, and feelings towards things; physical and psychological recovery; adaptive behaviours; and improvement of anxiety and depression.21 A randomized trial involving 24 elderly patients with essential hypertension provided evidence that forest bathing has therapeutic effects on hypertension and induces inhibition of the renin-angiotensin system and inflammation.22
Natural Medicines for Heart Health
 Fish Oils
Fish Oils
Omega‑3 fatty acid supplementation has been demonstrated to improve cardiovascular measures and outcomes. A meta-analysis of 13 randomized controlled trials involving 127,477 participants concluded that omega‑3 supplementation lowers the risk of myocardial infarction, coronary heart disease (CHD) death, total CHD, cardiovascular disease (CVD) death, and total CVD.23 A meta-analysis examining 11 randomized trial for 100,609 patients showed omega‑3 fatty acids had a statistically significant reduction in mortality due to cardiovascular issues (RR = 0.937 ; 95 % CI: 0.88 to 0.98; p = 0.018).24 Recently, another meta-analysis and metaregression of interventional trials involving 40 studies with a combined 135,267 participants concluded that EPA and DHA supplementation was associated with a statistically significant (p < 0.001) lower risk of CHD events and myocardial infarction (MI) in a dose-dependent fashion, where each additional 1 g/d was associated with a significant risk reduction of 9.0%. This meta-analysis also found a significant reduction in the risk of CVD (a 35% reduction in the risk of fatal MI, and a 9% reduction in the risk of CHD mortality).25
A meta-analysis examining 171 randomized, placebo controlled, blinded clinical trials aimed to quantify the effect of supplements containing EPA and DHA on risk factors for cardiovascular disease. Compared with control, EPA and DHA supplements produced significant reductions of triglycerides of 0.368 mmol/L (95% CI: −0.427 to −0.309), systolic blood pressure of 2,195 mmHg (95% CI: −3,172 to −1,217), diastolic blood pressure of 1.08 mmHg (95% CI: −1,716 to −0.444), heart rate of 1.37 bpm (95% CI: −2.41 to −0.325) and C‑reactive protein of 0.343 mg/L (95% CI: −0.454 to −0.232).26
Current evidence from multiple studies suggest that a higher dose of omega‑3 oils (2–4 g/d of combined EPA and DHA) appears to be safe and to reduce CVD events.27
Garlic
A 12-week randomized controlled trial involving 62 coronary heart patients with hyperhomocysteinemia resulted in subjects in the garlic allicin group (40 mg three times per day) showing significant decreases in carotid artery intima-media thickness, plasma homocysteine levels, total cholesterol, and triglycerides (p < 0.05). The decreases in the allicin group were significantly greater than those in the control group (all p < 0.01).28
A randomized, placebo-controlled, clinical trial of 56 patients with cardiovascular disease investigated the effect of garlic on the rate of atherosclerosis as measured by the carotid artery intima-media thickness (CIMT). After three months, CIMT values of the patients receiving garlic powder tablets (1200 µg allicin twice daily) had minor variations (0.009 ± 0.007 mm reduction from baseline), while in the placebo group, an increase in CIMT values was observed (0.04 ± 0.01 mm increase from baseline). After three months of treatment, mean CIMT difference from baseline was significantly different between the two groups (p < 0.001).29
 A meta-analysis of 12 trials involving adults with hypertension confirmed that garlic intervention, compared to the control, significantly lowered systolic blood pressure by 8.32 ± 1.93 mmHg (p < 0.00001), and diastolic blood pressure by 5.48 ± 1.92 mmHg (p < 0.00001). This decrease in blood pressure was associated with a 16–40% risk reduction of cardiovascular events such as heart attack and stroke.30
A meta-analysis of 12 trials involving adults with hypertension confirmed that garlic intervention, compared to the control, significantly lowered systolic blood pressure by 8.32 ± 1.93 mmHg (p < 0.00001), and diastolic blood pressure by 5.48 ± 1.92 mmHg (p < 0.00001). This decrease in blood pressure was associated with a 16–40% risk reduction of cardiovascular events such as heart attack and stroke.30
Also, in a systematic review and meta-analysis including 33 studies and a total of 1,273 individuals, the serum concentration of TC, LDL, TG, HDL, fasting blood glucose, and HbA1C showed significant improvements (p = 0.001) in the whole garlic supplementation group (500 mg–20,000 mg) versus the placebo group.31
Resveratrol
A randomized, double-blind, placebo-controlled trial involving 71 individuals with new diagnosis of dyslipidemia found that the individuals in the resveratrol group (100 mg/d) showed a significant decrease in total cholesterol (p = 0.04) and triglyceride (p = 0.04) concentrations compared with the placebo group.32
In a randomized controlled clinical trial involving 85 patients with coronary artery disease (stable angina pectoris—FC II), 55 patients in the comparison group were prescribed the standard therapy (β‑blockers, statins, aspirin) and the remaining 30 patients in the research group were prescribed the standard therapy plus resveratrol (100 mg). After two months, left ventricular ejection fraction significantly improved, by 9.7% in the research group and by 3.2% in the comparison group. Among other cardioprotective measures, the resveratrol group had significantly reduced numbers of premature atrial contractions and premature ventricular contractions.33
Conclusion
Naturopathic approaches to heart health include many evidence-based approaches including diet, lifestyle modification, and natural-medicine supplementation. The inclusion of multiple interventions is the ideal way to address heart health from a holistic standpoint and will likely yield additive benefits.
References :
[1] Swain, D.P. “The water-tower analogy of the cardiovascular system.” Advances in Physiology Education, Vol. 24, No. 1 (2000): 43–50.
[2] Koutroumpi, M., C. Pitsavos, and C. Stefanadis. “The role of exercise in cardiovascular rehabilitation: A review.” Acta Cardiologica, Vol. 63, No. 1 (2008): 73–79.
[3] Magyar, K., R. Halmosi, A. Palfi, G. Feher, L. Czopf, A. Fulop, I. Battyany, et al. “Cardioprotection by resveratrol: A human clinical trial in patients with stable coronary artery disease.” Clinical Hemorheology and Microcirculation, Vol. 50, No. 3 (2012): 179–187.
[4] Dinu, M., R. Abbate, G.F. Gensini, A. Casini, and F. Sofi. “Vegetarian, vegan diets and multiple health outcomes: A systematic review with meta-analysis of observational studies.” Critical Reviews in Food Science and Nutrition, Vol. 57, No. 17 (2017): 3640–3649.
[5] Magyar, K., R. Halmosi, A. Palfi, G. Feher, L. Czopf, A. Fulop, I. Battyany, et al. “Cardioprotection by resveratrol.”
[6] Soltani, S., M.J. Chitsazi, and A. Salehi-Abargouei. “The effect of dietary approaches to stop hypertension (DASH) on serum inflammatory markers: A systematic review and meta-analysis of randomized trials.” Clinical Nutrition, Vol. 37, No. 2 (2018): 542–550.
[7] Gallucci, G., A. Tartarone, R. Lerose, A.V. Lalinga, and A.M. Capobianco. “Cardiovascular risk of smoking and benefits of smoking cessation.” Journal of Thoracic Disease, Vol. 12, No. 7 (2020): 3866–3876.
[8] Huffman, J.C., S.R. Legler, and J.K. Boehm. “Positive psychological well-being and health in patients with heart disease: A brief review.” Future Cardiology, Vol. 13, No. 5 (2017): 443–450.
[9] Rozanski, A., C. Bavishi, L.D. Kubzansky, and R. Cohen. “Association of optimism with cardiovascular events and all-cause mortality: A systematic review and meta-analysis.” JAMA Network Open, Vol. 2, No. 9 (2019): e1912200.
[10] Kim, E.S., K.A. Hagan, F. Grodstein, D.L. DeMeo, I. De Vivo, and L.D. Kubzansky. “Optimism and cause-specific mortality: A prospective cohort study.” American Journal of Epidemiology, Vol. 185, No. 1 (2017): 21–29.
[11] Jackowska, M., J. Brown, A. Ronaldson, and A. Steptoe. “The impact of a brief gratitude intervention on subjective well-being, biology and sleep.” Journal of Health Psychology, Vol. 21, No. 10 (2016): 2207–2217.
[12] Carrillo, A., M. Rubio-Aparicio, G. Molinari, Á. Enrique, J. Sánchez-Meca, and R.M. Baños. “Effects of the Best Possible Self intervention: A systematic review and meta-analysis.” PloS One, Vol. 14, No. 9 (2019): e0222386.
[13] Steffen, P.R., and M.J. Larson. “A brief mindfulness exercise reduces cardiovascular reactivity during a laboratory stressor paradigm.” Mindfulness, Vol. 6 (2015): 803–811.
[14] Crnko, S., B.C. Du Pré, J.P.G. Sluijter, and L.W. Van Laake. “Circadian rhythms and the molecular clock in cardiovascular biology and disease.” Nature Reviews. Cardiology, Vol. 16, No. 7 (2019): 437–447.
[15] Man, A.W.C., H. Li, and N. Xia. “Circadian rhythm: Potential therapeutic target for atherosclerosis and thrombosis.” International Journal of Molecular Sciences, Vol. 22, No. 2 (2021): 676.
[16] Morris, C.J., T.E. Purvis, K. Hu, and F.A.J.L. Sheer “Circadian misalignment increases cardiovascular disease risk factors in humans.” Proceedings of the National Academy of Sciences of the United States of America, Vol. 113, No. 10 (2016): E1402–E1411.
[17] Laukkanen, J.A., T. Laukkanen, and S.K. Kunutsor. “Cardiovascular and other health benefits of sauna bathing: A review of the evidence.” Mayo Clinic Proceedings, Vol. 93, No. 8 (2018): 1111–1121.
[18] Kohara, K., Y. Tabara, M. Ochi, Y. Okada, M. Ohara, T. Nagai, Y. Ohyagi, and M. Igase. “Habitual hot water bathing protects cardiovascular function in middle-aged to elderly Japanese subjects.” Scientific Reports, Vol. 8, No. 1 (2018): 8687.
[19] Laukkanen, T., H. Khan, F. Zaccardi, and J.A. Laukkanen. “Association between sauna bathing and fatal cardiovascular and all-cause mortality events.” JAMA Internal Medicine, Vol. 175, No. 4 (2015): 542–548.
[20] Laukkanen, T., S.K. Kunutsor, F. Zaccardi, E. Lee, P. Willeit, H. Khan, and J.A. Laukkanen. “Acute effects of sauna bathing on cardiovascular function.” Journal of Human Hypertension, Vol. 32, No. 2 (2018): 129–138.
[21] Wen, Y., Q. Yan, Y. Pan, X. Gu, and Y. Liu. “Medical empirical research on forest bathing (Shinrin-yoku): A systematic review.” Environmental Health and Preventive Medicine, Vol. 24, No. 1 (2019): 70.
[22] Mao, G.‑X., Y.‑B. Cao, X.‑G. Lan, Z.‑H. He, Z.‑M. Chen, Y.‑Z. Wang, X.‑L. Hu, et al. “Therapeutic effect of forest bathing on human hypertension in the elderly.” Journal of Cardiology, Vol. 60, No. 6 (2012): 495–502.
[23] Hu, Y., F.B. Hu, and J.E. Manson. “Marine omega-3 supplementation and cardiovascular disease: An updated meta-analysis of 13 randomized controlled trials involving 127,477 participants.” Journal of the American Heart Association, Vol. 8, No. 19 (2019): e013543.
[24] Cabiddu, M.F., A. Russi, L. Appolloni, D. Mengato, and M. Chiumente. “Omega-3 for the prevention of cardiovascular diseases: meta-analysis and trial-sequential analysis.” European Journal of Hospital Pharmacy, Published Online First: 16 June 2020.
[25] Bernasconi, A.A., M.M. Wiest, C.J. Lavie, R.V. Milani, and J.A. Laukkanen. “Effect of omega-3 dosage on cardiovascular outcomes: An updated meta-analysis and meta-regression of interventional trials.” Mayo Clinic Proceedings, Vol. 96, No. 2 (2021): 304–313.
[26] AbuMweis, S., S. Jew, R. Tayyem, and L. Agraib. “Eicosapentaenoic acid and docosahexaenoic acid containing supplements modulate risk factors for cardiovascular disease: A meta-analysis of randomised placebo-control human clinical trials.” Journal of Human Nutrition and Dietetics, Vol. 31, No. 1 (2018): 67–84.
[27] Elagizi, A., C.J. Lavie, E. O’Keefe, K. Marshall, J.H. O’Keefe, and R.V. Milani. “An update on omega‑3 polyunsaturated fatty acids and cardiovascular health.” Nutrients, Vol. 13, No. 1 (2021): 204.
[28] Liu, D.‑S., S.‑L. Wang, J.‑M. Li, E.‑S. Liang, M.‑Z. Yang, and W. Gao. “Allicin improves carotid artery intima-media thickness in coronary artery disease patients with hyperhomocysteinemia.” Experimental and Therapeutic Medicine, Vol. 14, No. 2 (2017): 1722–1726.
[29] Mahdavi-Roshan, M., A. Zahedmehr, A. Mohammad‑Zadeh, H.‑R. Sanati, F. Shakerian, A. Firouzi, R. Kiani, and J. Nasrollahzadeh. “Effect of garlic powder tablet on carotid intima-media thickness in patients with coronary artery disease: a preliminary randomized controlled trial.” Nutrition and Health, Vol. 22, No. 2 (2013): 143–155.
[30] Ried, K. “Garlic lowers blood pressure in hypertensive subjects, improves arterial stiffness and gut microbiota: A review and meta-analysis.” Experimental and Therapeutic Medicine, Vol. 19, No. 2 (2020): 1472–1478.
[31] Shabani, E., K. Sayeremi, and M. Mohammadpour. “The effect of garlic on lipid profile and glucose parameters in diabetic patients: A systematic review and meta-analysis.” Primary Care Diabetes, Vol. 13, No. 1 (2019): 28–42.
[32] Simental-Mendía, L.E., and F. Guerrero‑Romero. “Effect of resveratrol supplementation on lipid profile in subjects with dyslipidemia: A randomized double-blind, placebo-controlled trial.” Nutrition, Vol. 58 (2019): 7–10.
[33] Chekalina, N.I. “Resveratrol has a positive effect on parameters of central hemodynamics and myocardial ischemia in patients with stable coronary heart disease.” Wiadomosci Lekarskie, Vol. 70, No. 2, Pt. 2 (2017): 286–291.