Related Articles
- 17 Aug 16
- 27 Apr 22
One of the key tenants of naturopathic medicine is education. In fact, one of the guiding principles of Naturopathic Medicine is Doctor as Teacher . This principle highlights the empowering nature of naturopathic medicine. A naturopathic doctor simply provides the tools, education, and resources for each patient to work on their own healing.
- 23 Dec 16
Dies ist Teil 2 unseres zweiteiligen Artikels zu Möglichkeiten der Geburtenkontrolle neben der „Pille“.
Teil 1 behandelte die Hormon- und Kupferspiralen. Teil 2 deckt den Ring, das Pflaster, das Diaphragma, die Kondome und die Rhythmusmethode ab. - 17 Aug 16
- 11 Sep 14
 A new article was recently published that described naturopathic practice at 4 of the 8 accredited North American naturopathic academic institutions [1]. The study includes an analysis of over 300,000 patient visits over 5 years, making it the largest study of its kind. It is unavoidable that the public asks: what is the difference between a Naturopathic Doctor and a Medical Doctor? The MD is certainly the more common medical degree and treatments are generally covered by the government or through insurance.
A new article was recently published that described naturopathic practice at 4 of the 8 accredited North American naturopathic academic institutions [1]. The study includes an analysis of over 300,000 patient visits over 5 years, making it the largest study of its kind. It is unavoidable that the public asks: what is the difference between a Naturopathic Doctor and a Medical Doctor? The MD is certainly the more common medical degree and treatments are generally covered by the government or through insurance. - 22 Dec 15
 According to Statistics Canada, results from the 2009 to 2011 Canadian Health Measures Survey (CHMS) indicate that 1 in 5 Canadian adults aged 18 to 79 had metabolic syndrome. Metabolic Syndrome, also known as Syndrome X, Insulin Resistance Syndrome, or Mets refers to a cluster of conditions that occur together. These conditions include high blood pressure, high blood sugar levels, excess body fat around the waist or mid-central obesity, and abnormal cholesterol levels.
According to Statistics Canada, results from the 2009 to 2011 Canadian Health Measures Survey (CHMS) indicate that 1 in 5 Canadian adults aged 18 to 79 had metabolic syndrome. Metabolic Syndrome, also known as Syndrome X, Insulin Resistance Syndrome, or Mets refers to a cluster of conditions that occur together. These conditions include high blood pressure, high blood sugar levels, excess body fat around the waist or mid-central obesity, and abnormal cholesterol levels. - 06 Oct 16
- 11 Aug 15
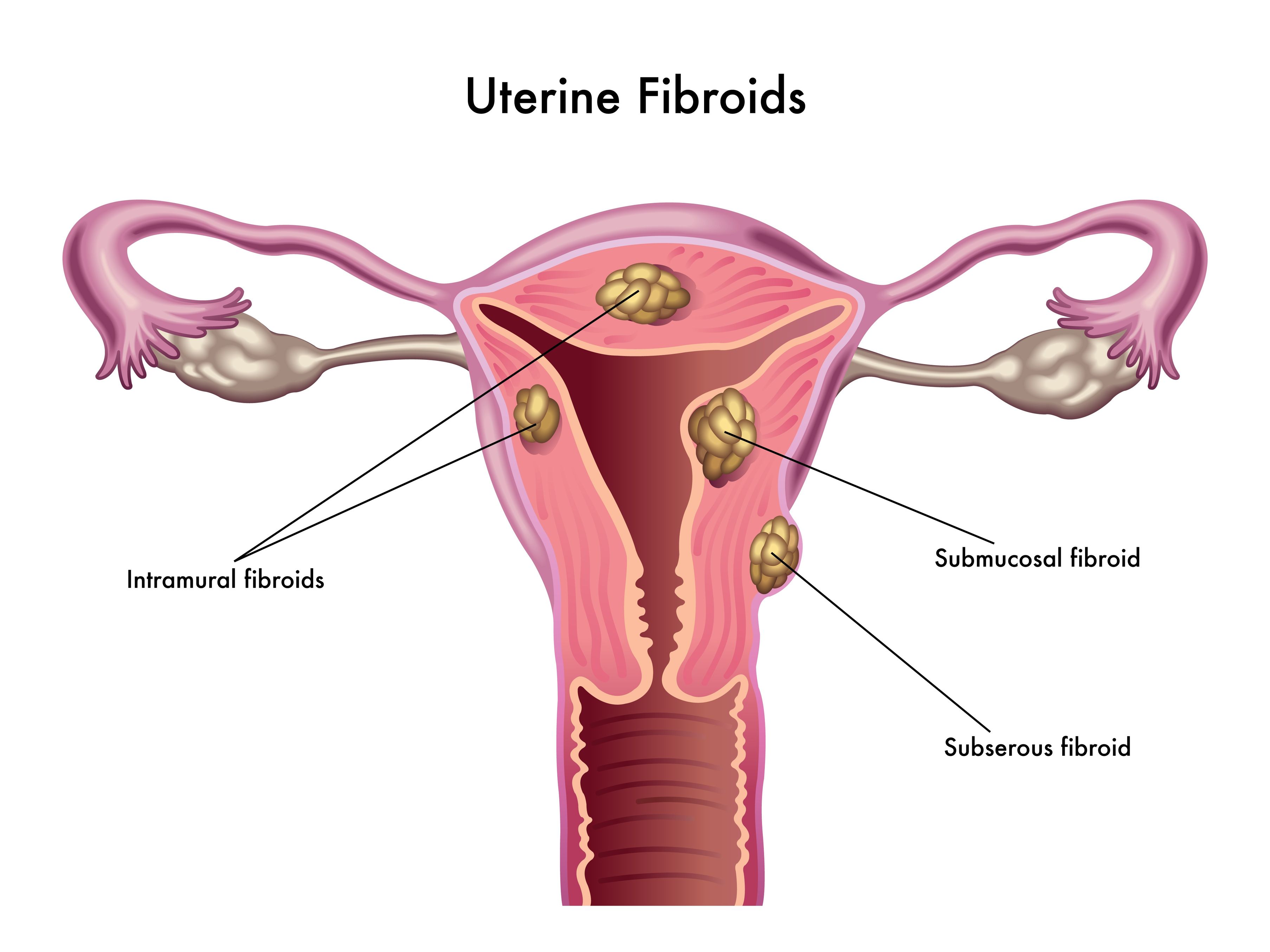
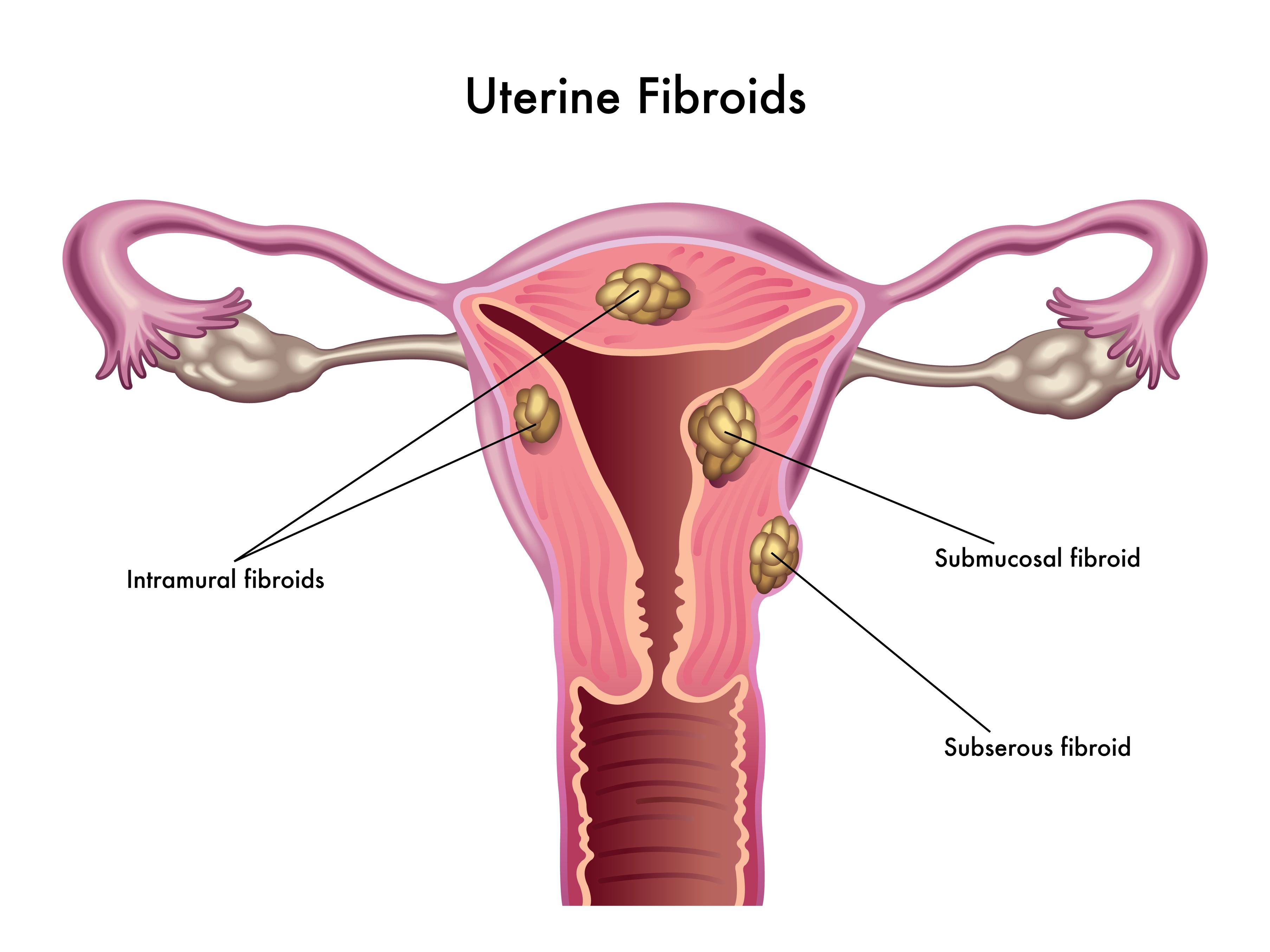 Uterine fibroids (also known as leiomyomas) are solid pelvic tumors composed of connective tissue and muscle [1]. Leiomyomas vary in terms of size, shape, and location; if one leiomyoma is discovered chances are multiple exist. Leiomyomas are either submucosal (under the endometrium), intramural (within the uterine wall), or subserosal (in the outer wall of the uterus).
Uterine fibroids (also known as leiomyomas) are solid pelvic tumors composed of connective tissue and muscle [1]. Leiomyomas vary in terms of size, shape, and location; if one leiomyoma is discovered chances are multiple exist. Leiomyomas are either submucosal (under the endometrium), intramural (within the uterine wall), or subserosal (in the outer wall of the uterus). - 02 Nov 16
- 19 Jan 17
- 31 May 19
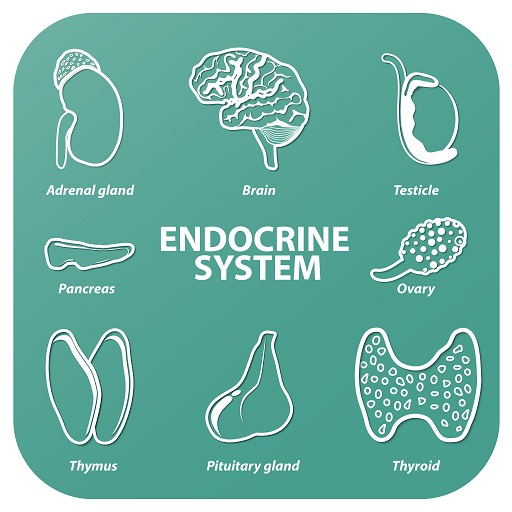
Have you ever wondered how your body is able to regulate its metabolism, mood, growth, temperature, heart rate, and even fertility?
- 03 Dec 14
 Concussions are the most common form of traumatic brain injury. Thousands of young people under the age of 19 are treated every year in hospital emergency rooms for concussions related to sports or other leisure activities. Concussions are most commonly caused by blows to the head, including car and bike accidents, or falls. Effects of concussions are usually temporary, but can include bothersome symptoms like headaches, problems concentrating, forgetfulness, and can also impact functions of balance and coordination.
Concussions are the most common form of traumatic brain injury. Thousands of young people under the age of 19 are treated every year in hospital emergency rooms for concussions related to sports or other leisure activities. Concussions are most commonly caused by blows to the head, including car and bike accidents, or falls. Effects of concussions are usually temporary, but can include bothersome symptoms like headaches, problems concentrating, forgetfulness, and can also impact functions of balance and coordination. - 10 Mar 18
Prenatal genetic testing is used to determine if a fetus has, or is at risk of developing, a genetic disorder. These disorders are caused by changes, often deletions or duplications, in fetal DNA and chromosomes. Two main types of testing often performed are screening and diagnosis. Screening tests typically look for aneuploidy—an abnormal number of chromosomes
- 13 Feb 16
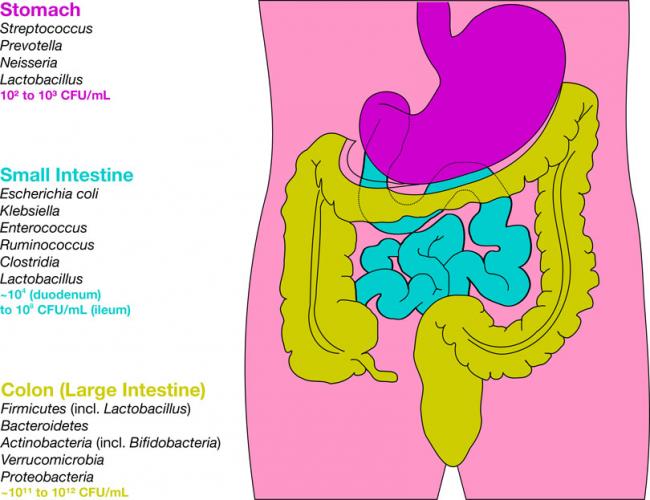
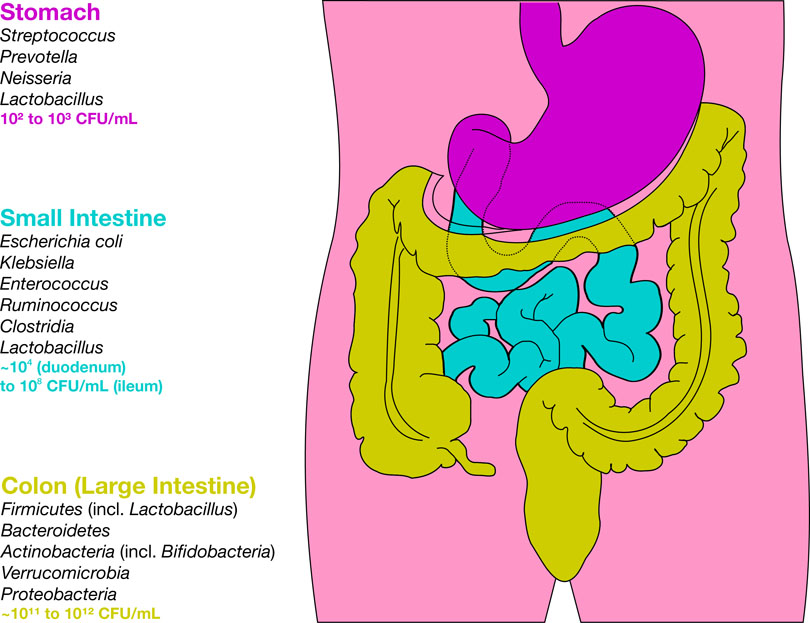 Small intestinal bacterial overgrowth (SIBO) is characterized by an overgrowth of various types of bacteria in the small intestine, bacteria which are largely only found in the colon. SIBO was initially thought of as a rare condition; however, it is now recognized as a more prevalent digestive disorder than previously acknowledged. A meta-analysis has shown the prevalence of SIBO to be approximately 64% among patients with irritable bowel syndrome
Small intestinal bacterial overgrowth (SIBO) is characterized by an overgrowth of various types of bacteria in the small intestine, bacteria which are largely only found in the colon. SIBO was initially thought of as a rare condition; however, it is now recognized as a more prevalent digestive disorder than previously acknowledged. A meta-analysis has shown the prevalence of SIBO to be approximately 64% among patients with irritable bowel syndrome - 23 Dec 16
- 02 Jun 17
 Understanding your menstrual cycle involves more than just estimating your next period. Knowing your body and tracking your menstrual cycles can provide insight into your hormonal and reproductive health. You might be experiencing symptoms that we usually label as “normal,” when we should be calling them “common.”
Understanding your menstrual cycle involves more than just estimating your next period. Knowing your body and tracking your menstrual cycles can provide insight into your hormonal and reproductive health. You might be experiencing symptoms that we usually label as “normal,” when we should be calling them “common.” - 15 Jan 17
- 11 Mar 16
 Aging is not really about how long someone has been alive, but more about the decline in physical ability and health that tends to occur once a person reaches later life. Aging involves a variety of factors—including our genes, our environment, and infections with harmful viruses and bacteria. These factors—genetic, environmental, and biological—can overlap and cause us to begin the aging process, called “senescence,” which goes all the way down to the cellular level.
Aging is not really about how long someone has been alive, but more about the decline in physical ability and health that tends to occur once a person reaches later life. Aging involves a variety of factors—including our genes, our environment, and infections with harmful viruses and bacteria. These factors—genetic, environmental, and biological—can overlap and cause us to begin the aging process, called “senescence,” which goes all the way down to the cellular level. - 05 May 14
 Concussions are extremely common in our society — an estimated 75% of all people will experience one in their lifetime!The majority of people recover completely from concussions within a week or two; yet, for a considerable number of people, the negative effects can last for months and even years. Mood symptoms like anxiety, irritability, and depression coincide with physical symptoms like headaches, fatigue, nausea, and dizziness; added to that are cognitive symptoms like problems with memory, decision making, and concentration difficulties. This constellation of symptoms is known as postconcussion syndrome (PCS).
06 Sep 16
Concussions are extremely common in our society — an estimated 75% of all people will experience one in their lifetime!The majority of people recover completely from concussions within a week or two; yet, for a considerable number of people, the negative effects can last for months and even years. Mood symptoms like anxiety, irritability, and depression coincide with physical symptoms like headaches, fatigue, nausea, and dizziness; added to that are cognitive symptoms like problems with memory, decision making, and concentration difficulties. This constellation of symptoms is known as postconcussion syndrome (PCS).
06 Sep 16
Newsletter
Most Popular
- 09 Jul 15
- 13 Feb 16
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13