Related Articles
- 26 Feb 21
The kidneys are one of the body’s most important filtration systems and are sometimes overlooked until there is an issue. In traditional Chinese medicine, the kidneys are often referred to as the “root of life,” and they play an important role in overall vitality, especially as we age.
- 02 Nov 16
- 03 Feb 15
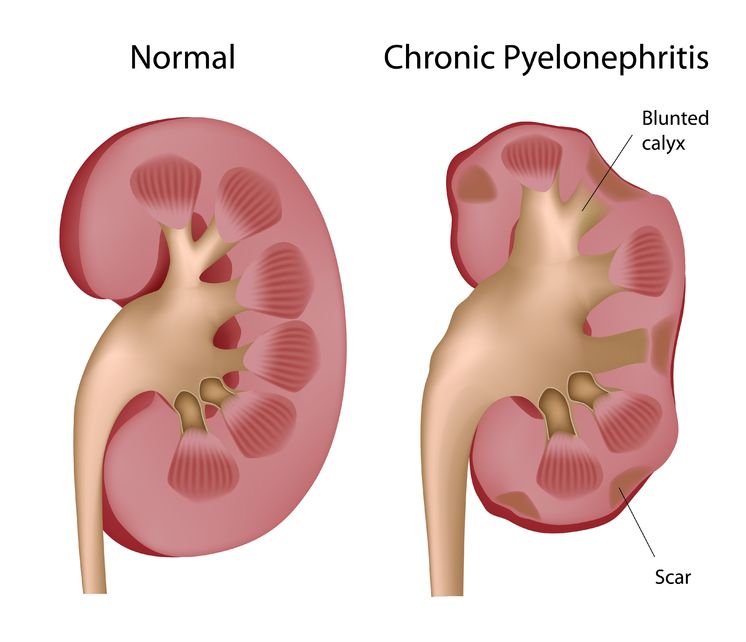
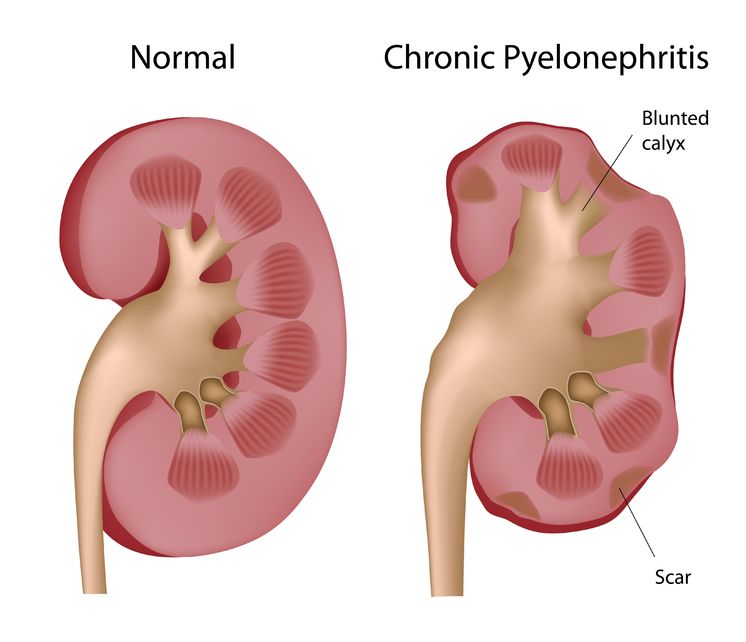 Pyelonephritis is the result of a progressive urinary tract infection, when a lower urinary infection travels upward into the upper urinary system. The lower urinary infections originate in the bladder and urethra, while the upper urinary infections involve the ureters and the kidneys. The kidneys filter the blood, so pyelonephritis can be potentially dangerous because an infection could then spread into the bloodstream.
Pyelonephritis is the result of a progressive urinary tract infection, when a lower urinary infection travels upward into the upper urinary system. The lower urinary infections originate in the bladder and urethra, while the upper urinary infections involve the ureters and the kidneys. The kidneys filter the blood, so pyelonephritis can be potentially dangerous because an infection could then spread into the bloodstream. - 04 Oct 17
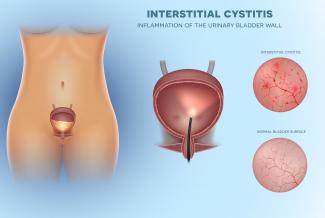
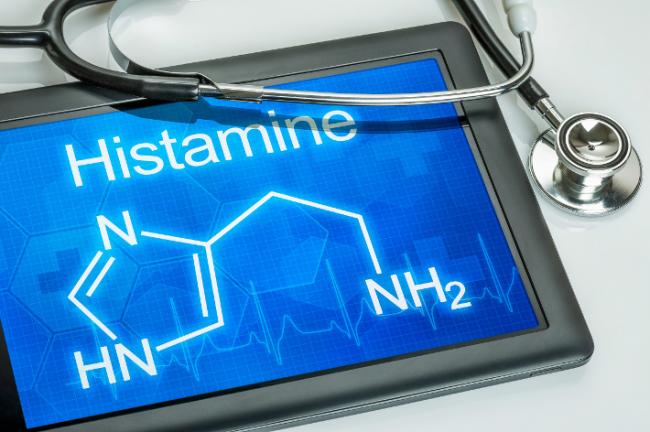
 Interstitial cystitis is a multifactorial condition and no single pathological process is present universally in patients with IC. It is thus important to determine the root causes of the individual’s symptoms, which commonly include bladder-wall dysfunction and permeability, urine acidity, and infection.
Interstitial cystitis is a multifactorial condition and no single pathological process is present universally in patients with IC. It is thus important to determine the root causes of the individual’s symptoms, which commonly include bladder-wall dysfunction and permeability, urine acidity, and infection. - 18 Mar 19
Over 50% of women will suffer from a urinary tract infection (UTI) during their lifetime. One-third to one-half of these women will have a recurrent UTI within one year.
- 04 Oct 17
 Interstitial cystitis (IC) is a long-term disorder of the bladder. The exact cause of IC is unknown. The function of the bladder is to store urine that it receives from the kidneys. You can think of the bladder as acting like a balloon made of muscle. It expands to hold large amounts of urine, and contracts to squeeze it out.
Interstitial cystitis (IC) is a long-term disorder of the bladder. The exact cause of IC is unknown. The function of the bladder is to store urine that it receives from the kidneys. You can think of the bladder as acting like a balloon made of muscle. It expands to hold large amounts of urine, and contracts to squeeze it out. - 05 Jul 19
- 18 Sep 18
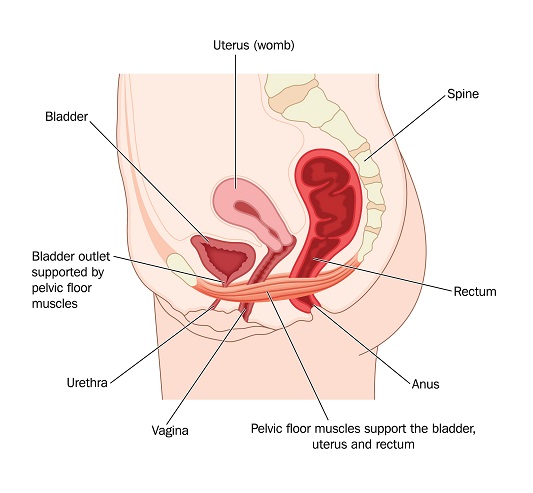
The urinary tract is part of the excretory system that removes wastes and unnecessary metabolites from the body to maintain homeostasis and biochemical balance. Made up of the kidneys, ureters, bladder, and urethra, the urinary tract is perceived to be sterile, except for the urethra.
- 31 May 19
The structure of the pelvic floor creates a support system for the pelvic organs. These muscles, composed by the pelvic diaphragm and elevator ani complex, form a sling around the urethra, distal vagina, and rectum.
- 01 Jul 13
$path = isset($_GET['q']) ? $_GET['q'] : '
';
$link = url($path, array('absolute' => TRUE));$nid = arg(1);
if ($nid == 201307){
?>download pdf
}
?>
Polycystic kidney disease (PKD) is a genetic disease in which multiple cysts grow on the kidneys. As the cysts expand in size, they impinge on the normal structure of the kidney, and there is a decrease in kidney function. In people with severe forms of the disease, this leads to a condition called end-stage renal disease (ESRD), which refers to such low kidney filtering function that dialysis and kidney transplantation become necessary.
Newsletter
Most Popular
- 27 Jan 21
- 03 Jan 14
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13