Related Articles
- 13 Apr 20
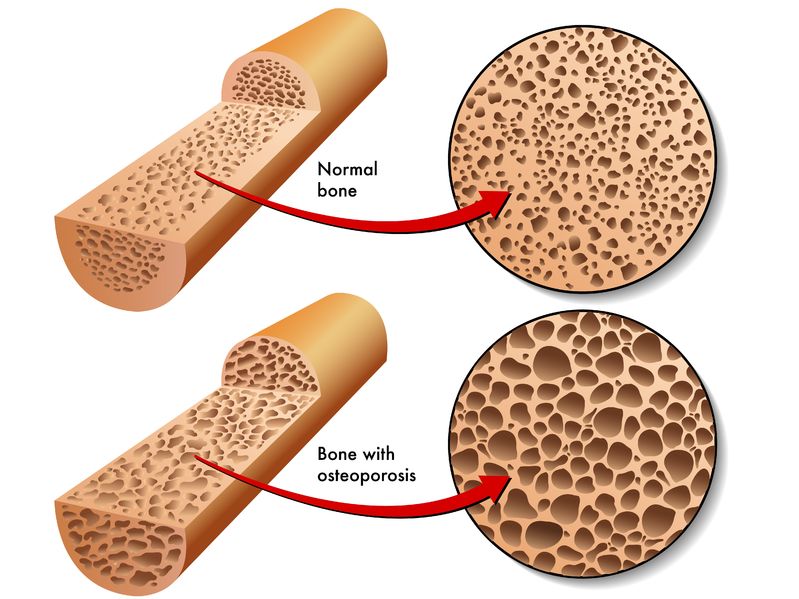
Bone is our main structural support system. It allows us to protect our vital organs, facilitates movement, and creates a scaffold for blood vessels and nerves. In additional to the structural functions, bone has important metabolic and endocrine functions as well.
- 17 Dec 19
Collagen peptides have seemingly appeared out of nowhere. They are being advertised on social media, can be found on the covers of magazines… even my hairdresser has been talking about how she adds collagen peptides to her smoothie! But what are collagen peptides? Why is everyone adding this powder to their coffee, smoothies, or breakfast oatmeal bowl? And the real question is: Should you be adding collagen peptides to your diet as well?
- 17 Jul 16
- 03 May 17
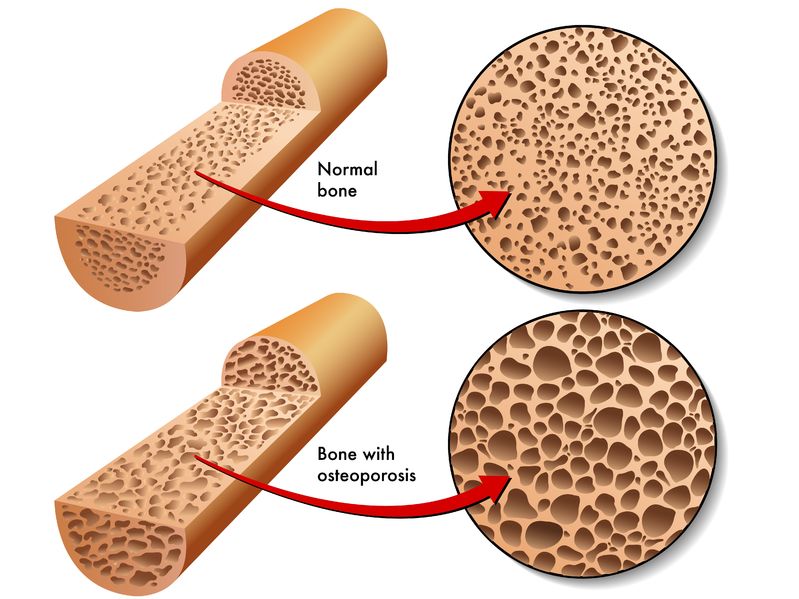
 Back pain is extremely common and has been experienced by almost everyone at one point in life. The official name for low back pain is lumbago, and it is literally defined as pain in the lower back. There are many possible causes for back pain, and often it is not even possible to identify a specific cause. If this is the case, it might be called nonspecific.
Back pain is extremely common and has been experienced by almost everyone at one point in life. The official name for low back pain is lumbago, and it is literally defined as pain in the lower back. There are many possible causes for back pain, and often it is not even possible to identify a specific cause. If this is the case, it might be called nonspecific. - 09 Nov 15
- 09 Jul 15
 Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank.
Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank. - 22 Dec 16
- 09 Nov 15
 This action that berberine has on AMPK is one of the main reasons that interest in berberine’s effects on blood sugar management have been studied. AMPK activation is one the main mechanisms of action of the popular diabetes medication metformin (Glucophage). In human trials berberine has been extremely impressive in this regard. Let’s take a look at some of the studies.
This action that berberine has on AMPK is one of the main reasons that interest in berberine’s effects on blood sugar management have been studied. AMPK activation is one the main mechanisms of action of the popular diabetes medication metformin (Glucophage). In human trials berberine has been extremely impressive in this regard. Let’s take a look at some of the studies. - 28 Feb 19
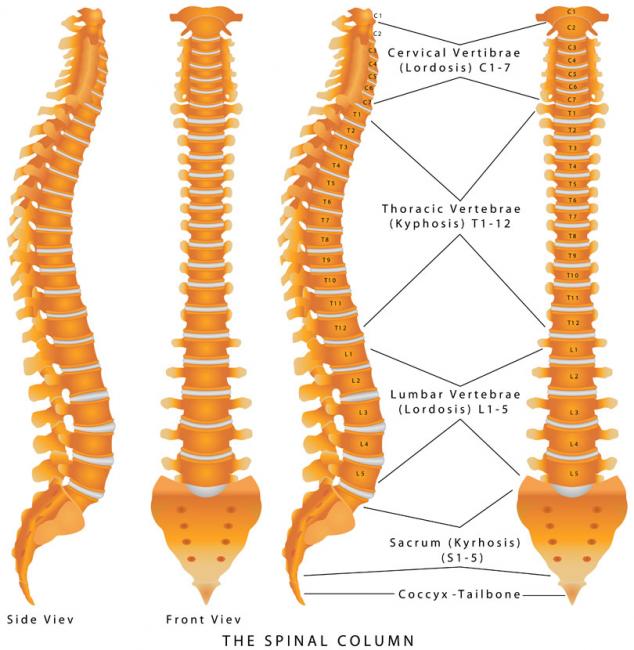
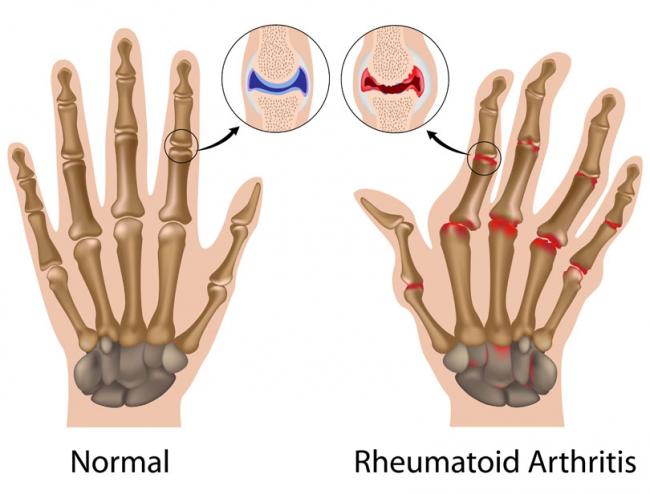
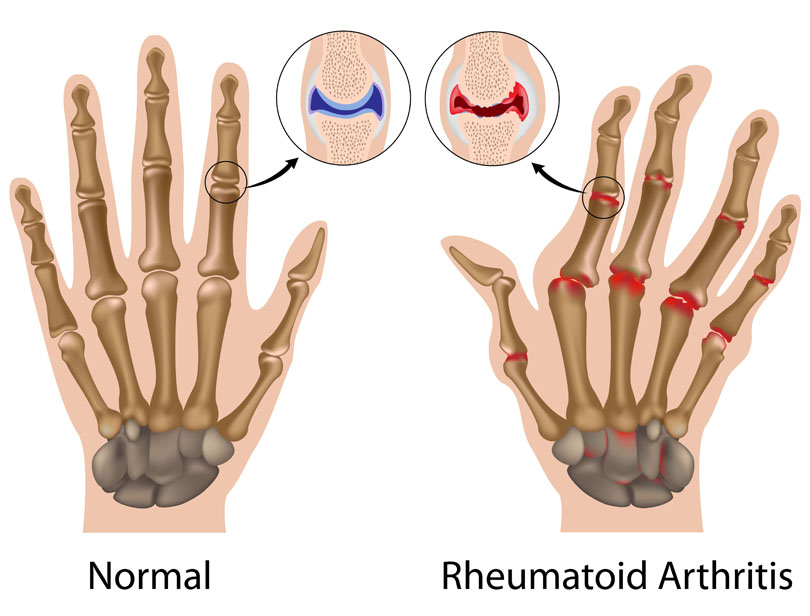
Chronic pain is a significant health issue, and it is estimated that one-half of those suffering with chronic pain have been suffering for longer than 10 years.[1] An estimated 54.4 million North Americans have been diagnosed with various arthritic disorders,[2] conditions that are typically treated with nonsteroidal anti-inflammatory drugs (NSAIDs).
- 11 Mar 16
 Walk down a busy street and you’ll see some atrocious body language and posture. Most people are hunched over, head down, eyebrows furrowed, and probably typing away on their cell phones. Anybody who is sitting is almost guaranteed to be hunched over: driving, eating, talking, on the phone, going to the toilet, working at a desk, studying, etc.
Walk down a busy street and you’ll see some atrocious body language and posture. Most people are hunched over, head down, eyebrows furrowed, and probably typing away on their cell phones. Anybody who is sitting is almost guaranteed to be hunched over: driving, eating, talking, on the phone, going to the toilet, working at a desk, studying, etc. - 13 Apr 17
- 17 May 18
Magnesium is the fourth most-abundant mineral in the human body, and is essential for the hundreds of metabolic and hormonal reactions occurring daily. It is generally known to be a component of bone formation (partnered with calcium), and is gaining more interest as a sleep aid due to its natural muscle relaxant properties.
- 19 Jun 19
 Many of us are aware that exercise is an important part of creating a healthy and balanced life. And yet, many more of us are so quick to create excuses and avoid the effort it takes to get our bodies moving. The truth of the matter is, there is no pill that can replicate what exercise can do for the human body. And like everything else that we do to occupy our time, if it is important enough to us, we will make it a priority. Exercise is an important part of managing every health concern, and here are three of my favourites.
Many of us are aware that exercise is an important part of creating a healthy and balanced life. And yet, many more of us are so quick to create excuses and avoid the effort it takes to get our bodies moving. The truth of the matter is, there is no pill that can replicate what exercise can do for the human body. And like everything else that we do to occupy our time, if it is important enough to us, we will make it a priority. Exercise is an important part of managing every health concern, and here are three of my favourites. - 16 Jun 21
Protocols in naturopathic practice are designed to help increase health span while taking into consideration the extent of disease, a variety of modalities or tools of applicability, and patient choice and values; however, exercise prescriptions stand out as part of a foundational approach nearly ubiquitous and necessary for almost everyone.
- 03 Jan 14
$path = isset($_GET['q']) ? $_GET['q'] : '
';
$link = url($path, array('absolute' => TRUE));$nid = arg(1);
if ($nid == 201401){
?>download pdf
}
?> Turmeric is a golden-color spice widely used in South Eastern and Middle Eastern cooking. Besides being a popular spice, it is also an important herb used in many disciplines of medicine. The medicinal use of turmeric dates back to 4000 years ago in India. It takes on many different names: Indian saffron, haldi, rhizoma curcumae (jiang huang), asterre merite.
01 May 21
Turmeric is a golden-color spice widely used in South Eastern and Middle Eastern cooking. Besides being a popular spice, it is also an important herb used in many disciplines of medicine. The medicinal use of turmeric dates back to 4000 years ago in India. It takes on many different names: Indian saffron, haldi, rhizoma curcumae (jiang huang), asterre merite.
01 May 21Acupuncture is a traditional therapy that has been used for thousands of years for the treatment of various ailments such as pain, fertility concerns, low energy, mood swings, and even colds and flu. It involves the insertion of very fine needles at specific points on the body to promote healing through the stimulation and circulation of “Qi.”
05 Jun 1706 Nov 14Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, is a neuromuscular disease that is characterized by progressive nerve cell death leading to muscle weakness, paralysis and severe physical dysfunction. Approximately 2,500-3,000 Canadians currently live with this fatal disease.
11 Mar 1618 Jun 19We know that exercise is good for us. It helps with our heart health, our blood sugar, our thyroid, our sleep, and our ability to manage stress. It helps with almost everything relating to our health and is probably one of the most important factors for good health, if not the most important.
Newsletter
Most Popular
- 27 Jan 21
- 06 Oct 16
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13