Related Articles
- 15 Sep 23
Acupuncture shows promise in reducing cancer treatment side effects in small studies. Further research with larger populations and funding could boost its role in Western cancer care. With its history, minimal side effects, and energy benefits, acupuncture may become a common recommendation for cancer recovery.
- 17 Dec 19
Energy medicine comes in many forms, defined as
anything that works on the energetic biofield of the
human body, also known as the aura. Focusing on
this aspect of health in turn has a ripple effect into
other aspects including emotional, mental, physical,
and even spiritual. I would like to focus this article
specifically on reiki of the Usui origin. - 08 Jul 20
As the COVID-19 pandemic seemed to shut down the world, grocery stores, or at least what was left on the shelves at grocery stores, became an indicator of where people were at in their experience of the stressful event.
- 01 Feb 14
$path = isset($_GET['q']) ? $_GET['q'] : '
';
$link = url($path, array('absolute' => TRUE));$nid = arg(1);
if ($nid == 201402){
?>download pdf
}
?> Many readers will be aware of an ongoing public debate regarding the validity of naturopathic medicine. The debate often centers on the existence of evidence to support the safety and effectiveness of naturopathic medicine. In this article, we throw new light on the state of naturopathic medicine research and highlight the oft-overlooked body of evidence that already exists.
02 Jul 14
Many readers will be aware of an ongoing public debate regarding the validity of naturopathic medicine. The debate often centers on the existence of evidence to support the safety and effectiveness of naturopathic medicine. In this article, we throw new light on the state of naturopathic medicine research and highlight the oft-overlooked body of evidence that already exists.
02 Jul 14 Today more people than ever are seeking naturopathic care, especially for long standing conditions including but not limited to anxiety, diabetes, depression and cardiovascular disease. What many people may not realize is that naturopathic doctors are also well trained in treating acute injuries as well as more chronic cases of pain caused by previous injuries or other conditions including osteoarthritis. Dealing with pain, whether from a recent injury or from a long standing condition can be very difficult.
08 Jun 1503 May 17
Today more people than ever are seeking naturopathic care, especially for long standing conditions including but not limited to anxiety, diabetes, depression and cardiovascular disease. What many people may not realize is that naturopathic doctors are also well trained in treating acute injuries as well as more chronic cases of pain caused by previous injuries or other conditions including osteoarthritis. Dealing with pain, whether from a recent injury or from a long standing condition can be very difficult.
08 Jun 1503 May 17 Back pain is extremely common and has been experienced by almost everyone at one point in life. The official name for low back pain is lumbago, and it is literally defined as pain in the lower back. There are many possible causes for back pain, and often it is not even possible to identify a specific cause. If this is the case, it might be called nonspecific. 17 Jun 16
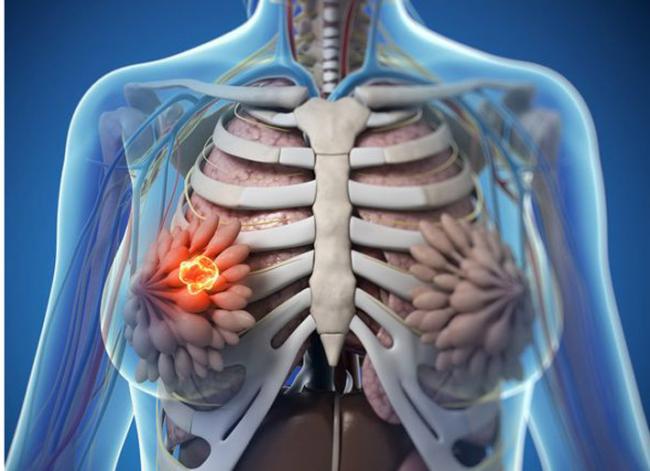
Back pain is extremely common and has been experienced by almost everyone at one point in life. The official name for low back pain is lumbago, and it is literally defined as pain in the lower back. There are many possible causes for back pain, and often it is not even possible to identify a specific cause. If this is the case, it might be called nonspecific. 17 Jun 16 The use of complementary medicine for the treatment of cancer and its side effects has skyrocketed in recent years. Complementary therapies refer to ones that are nonpharmaceutical in nature, and that have the potential to not only enhance quality of life, but also to reduce side effects of conventional therapy.09 Jul 15
The use of complementary medicine for the treatment of cancer and its side effects has skyrocketed in recent years. Complementary therapies refer to ones that are nonpharmaceutical in nature, and that have the potential to not only enhance quality of life, but also to reduce side effects of conventional therapy.09 Jul 15 Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank.06 Sep 1618 Jan 19
Whole-body cryotherapy (WBC) is a health promoting treatment that involves short exposures to air temperatures below −100°C [1]. WBC treatments last approximately 2-5 minutes and the frequency of treatments can vary based on the purpose of use. The patient is placed in a small cabin that emits a dry cold mist that is suctioned from a neighbouring liquid nitrogen tank.06 Sep 1618 Jan 19A large portion of people who see naturopathic doctors come with a chief concern of digestive issues. After months of scopes and bloodwork, they are often left without answers from their medical doctor and seek a new perspective. Other times, their diagnostic imaging tests reveal something significant, yet the medical system is still at a loss for treatment options.
22 Dec 1628 Feb 19Chronic pain is a significant health issue, and it is estimated that one-half of those suffering with chronic pain have been suffering for longer than 10 years.[1] An estimated 54.4 million North Americans have been diagnosed with various arthritic disorders,[2] conditions that are typically treated with nonsteroidal anti-inflammatory drugs (NSAIDs).
11 Sep 14 Detoxifying the body can be achieved in many ways. Essentially, the goal is to eliminate chemicals and environmental pollutants that place a toxic burden to our bodies that are responsible for the progression to many health concerns. Recent research has shown to find over 5 million chemicals in our environment, which have negative effects on the muscular, neurological, cardiovascular, and pulmonary systems in the body02 Oct 14
Detoxifying the body can be achieved in many ways. Essentially, the goal is to eliminate chemicals and environmental pollutants that place a toxic burden to our bodies that are responsible for the progression to many health concerns. Recent research has shown to find over 5 million chemicals in our environment, which have negative effects on the muscular, neurological, cardiovascular, and pulmonary systems in the body02 Oct 14 Mindfulness is the practice that cultivates paying attention on purpose, in the present moment, nonjudgmentally to our experience. It is not a belief or philosophy, but an awareness of the nature of the mind and our emotions. Mindfulness is often confused with meditation, and while the practices are interconnected, they have different origins.05 Aug 14
Mindfulness is the practice that cultivates paying attention on purpose, in the present moment, nonjudgmentally to our experience. It is not a belief or philosophy, but an awareness of the nature of the mind and our emotions. Mindfulness is often confused with meditation, and while the practices are interconnected, they have different origins.05 Aug 14 The term “dysmenorrhea” is commonly used to describe painful menstruation. Considered one of the most common conditions in women’s health, its effective treatment relies on determining and addressing the root cause. When the pain is due to a specific pelvic or systemic condition, it is referred to as “secondary dysmenorrhea”; in the absence of disease or physical abnormalities, menstrual pain is referred to as “primary dysmenorrhea”.15 Sep 1703 Jan 14
The term “dysmenorrhea” is commonly used to describe painful menstruation. Considered one of the most common conditions in women’s health, its effective treatment relies on determining and addressing the root cause. When the pain is due to a specific pelvic or systemic condition, it is referred to as “secondary dysmenorrhea”; in the absence of disease or physical abnormalities, menstrual pain is referred to as “primary dysmenorrhea”.15 Sep 1703 Jan 14$path = isset($_GET['q']) ? $_GET['q'] : '
';
$link = url($path, array('absolute' => TRUE));$nid = arg(1);
if ($nid == 201401){
?>download pdf
}
?> Chronic pain affects a large percentage of the general population on a daily or otherwise regular basis. It includes a variety of different conditions, such as osteoarthritis (“wear and tear” arthritis), rheumatoid arthritis, migraine, fibromyalgia, low-back pain, and even repetitive strain conditions such as various types of tendonitis and other injuries that do not heal properly.
18 Oct 19
Chronic pain affects a large percentage of the general population on a daily or otherwise regular basis. It includes a variety of different conditions, such as osteoarthritis (“wear and tear” arthritis), rheumatoid arthritis, migraine, fibromyalgia, low-back pain, and even repetitive strain conditions such as various types of tendonitis and other injuries that do not heal properly.
18 Oct 19According to Statistics Canada, 1 in 10 individuals between the ages of 12 and 44 experience chronic pain. Once traditional medicine has been helpful in the acute-pain stage (e.g. first aid, over-the-counter pain killers, heat/ice, etc.), modern medicine may leave individuals feeling lost when it comes to long-term management and reduction of chronic pain.
27 Sep 21Acupuncture is an ancient medicinal system in which fine needles are inserted into specific points on the body, with the purpose of managing disease and restoring function. Recent research has expanded our understanding of how acupuncture works on the body.
Newsletter
Most Popular
- 07 May 15
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13