Related Articles
- 11 Aug 17
- 15 Jun 21
Medium-chain triglycerides, or MCTs, have been popularized in the context of Bulletproof™ coffee or the ketogenic diet. MCTs and the keto diet have been investigated in the management of obesity, insulin resistance, , epilepsy, neurodegenerative conditions, and others.
- 29 Jan 21Adrenal fatigue affects individuals who suffer from a long stretch of physical, mental, environmental, or emotional stress. A “long stretch” can be defined as greater than three months. Adrenal fatigue can affect anyone, but individuals who are more likely to suffer from adrenal fatigue include single parents, individuals who are drug-dependent, those who have faced a life crisis or trauma, or those who have a stressful job circumstance.
- 09 Mar 20
Seasonal affective disorder (SAD) is a type of depression that is only present during the winter months. This differs from clinical depression, which has no seasonal pattern. SAD also tends to improve when the springtime occurs.
- 27 Sep 21
Throughout the ages, humans have searched for the Fountain of Youth. Today, the search for eternal youth continues; however, we are no longer looking for a hidden fountain but instead, for lifestyle, dietary, and technological hacks we can use in attempts to delay the aging process.
- 17 Dec 19
Sadness, hopelessness and loss of interest in previously interesting activities are the hallmark of a serious, well-known mood disorder commonly referred to as depression. The Diagnostic and Statistical Manual of Mental Disorders (DSM) defines the disorder based on specific emotions that one must feel for a set amount of time.
- 05 May 20
Coronavirus disease 2019 (COVID‑19) is a pandemic that has affected more than 200 countries all around the world, according to the World Health Organization. This disease outbreak, which started in January 2020, has shocked the world due to its uncontrollable spread and increasing death rate. Social isolation, reduced financial ability, and the lack of certainty about the future may cause symptoms of anxiety and depression in many individuals during this period. Amidst all this, many are worried about their own health status or the health of their loved ones.
- 12 Feb 20
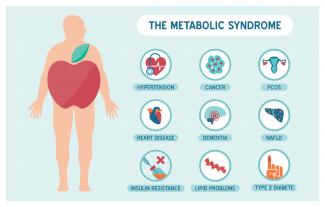
Metabolic syndrome is a cluster of risk factors that increase one’s chances of developing serious illnesses in the future. Metabolic syndrome doubles the chance of developing cardiovascular disease while increasing the risk of diabetes, fatty liver, and several types of cancers.[1][2]
- 09 Mar 20
The viruses that cause colds and the flu can be spread easily by coughing and sneezing. While there is no way to guarantee you won’t get sick this winter, there are things you can do to reduce the severity of your sickness.
- 10 Jun 20
Peripheral neuropathy is a common type of neuralgia, with diabetic neuropathy and postherpetic neuralgia being the most common types.
- 08 Jul 20
Anxiety is a very common mental-health disorder and can have implications on all aspects of one’s life. This may come from a variety of factors such as finances, relationships, health, and more. Anxiety lends itself well to natural treatments such as herbal medicine, supplements, and lifestyle modification
- 13 Apr 20
Itchy skin, dryness, redness, and cracking—uncomfortable signs of an eczema flare-up that can range from mild to having a significant impact on quality of life. Corticosteroid creams can do a fine job of targeting symptoms and inflammation associated with eczema, although below are some suggestions to get to the root cause and prevent future flare-ups.
- 09 Mar 20
Botanical medicine, or the study and use of plants as medicine, is one of my favourite healing modalities as a naturopathic doctor. I especially love using plants that are widely available and that people are familiar with. I find that knowing and feeling connected with and excited about any medicine I am taking seems to make it that much more effective.
- 10 Jun 20
In many countries around the world, alcoholic beverages are built into the culture and religion. We consume it as a form of celebration and a form of self-medication. But over the years, it takes a toll on our organ system that works to filter it out. Fatty liver disease is a growing concern in the Western hemisphere, especially as new diagnoses include people of normal body weights and people who don’t drink alcohol.
- 05 Jun 17
- 02 Jul 14
 Today more people than ever are seeking naturopathic care, especially for long standing conditions including but not limited to anxiety, diabetes, depression and cardiovascular disease. What many people may not realize is that naturopathic doctors are also well trained in treating acute injuries as well as more chronic cases of pain caused by previous injuries or other conditions including osteoarthritis. Dealing with pain, whether from a recent injury or from a long standing condition can be very difficult.
13 Apr 15
Today more people than ever are seeking naturopathic care, especially for long standing conditions including but not limited to anxiety, diabetes, depression and cardiovascular disease. What many people may not realize is that naturopathic doctors are also well trained in treating acute injuries as well as more chronic cases of pain caused by previous injuries or other conditions including osteoarthritis. Dealing with pain, whether from a recent injury or from a long standing condition can be very difficult.
13 Apr 15 The prevalence of overweight and obesity has skyrocketed in North America over recent years, and weight management strategies employed have had little widespread success. Both science and the public have been interested in natural and synthetic weight loss aids for decades, the most recent slimming agent being Garcinia cambogia (G. cambogia) and its extract (−)‑hydroxycitric acid (HCA).26 Feb 21
The prevalence of overweight and obesity has skyrocketed in North America over recent years, and weight management strategies employed have had little widespread success. Both science and the public have been interested in natural and synthetic weight loss aids for decades, the most recent slimming agent being Garcinia cambogia (G. cambogia) and its extract (−)‑hydroxycitric acid (HCA).26 Feb 21Long before February was declared “Heart Month” in Canada, “American Heart Month” in the United States, and “National Heart Month” in the United Kingdom, children and adults celebrated February 14 as a day of love and affection.
11 Aug 15 There is a new, growing interest in the field of male infertility, given the recent trends of declining conception over the past decade. The times are telling of families having fewer children, later in age and often having more difficulties with conception. Infertility can pose physical, psychological, financial and economic burden on individuals, the health care system and society.13 Apr 17
There is a new, growing interest in the field of male infertility, given the recent trends of declining conception over the past decade. The times are telling of families having fewer children, later in age and often having more difficulties with conception. Infertility can pose physical, psychological, financial and economic burden on individuals, the health care system and society.13 Apr 17
Newsletter
Most Popular
- 09 Jul 15
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13
- 17 Jun 13
- 17 Jun 13
- 17 Jun 13
- 01 Jul 13